Living with sleep apnea can be a significant challenge for older adults. As they age, the risk of developing this sleep disorder increases, causing interruptions in breathing during sleep and leading to a range of health issues. However, there are solutions available to help manage this condition and improve the quality of life for those who are affected. In this article, we will explore the challenges faced by older adults with sleep apnea and provide strategies and solutions to address this common issue.
Understanding Sleep Apnea
Sleep apnea is a common sleep disorder characterized by pauses in breathing or shallow breaths during sleep. These pauses can last for a few seconds to a minute and can occur multiple times throughout the night. There are three types of sleep apnea: obstructive sleep apnea (OSA), central sleep apnea (CSA), and complex sleep apnea syndrome (formerly known as mixed sleep apnea). OSA is the most prevalent form, accounting for about 84% of sleep apnea cases.
Prevalence in Older Adults
Sleep apnea is more prevalent in older adults, with the risk increasing with age. Studies have shown that around 20-30% of older adults have some form of sleep apnea. The prevalence is higher in males, individuals with obesity, and those with certain medical conditions. As the population continues to age, the impact of sleep apnea on older adults becomes increasingly significant.

Causes of Sleep Apnea
The causes of sleep apnea vary depending on the type. Obstructive sleep apnea occurs when the muscles in the throat fail to keep the airway open during sleep. Central sleep apnea is caused by a malfunction in the central nervous system, which fails to signal the muscles to breathe. The exact cause of complex sleep apnea syndrome is not fully understood, but it is thought to be a combination of both obstructive and central sleep apnea.
Identifying Sleep Apnea in Older Adults
Symptoms of Sleep Apnea
Recognizing the symptoms of sleep apnea is crucial for early intervention. Common symptoms include loud snoring, gasping for air during sleep, daytime sleepiness, morning headaches, dry mouth or sore throat upon waking up, and difficulty concentrating or remembering. Older adults may also experience nocturia (frequent urination at night) and mood changes.
Diagnosing Sleep Apnea
To get an accurate diagnosis, a sleep study is usually conducted. This can be done either in a sleep laboratory or at home using portable devices. The sleep study monitors various parameters such as breathing patterns, oxygen levels, and brain activity to determine the presence and severity of sleep apnea. It is important to consult with a healthcare professional to interpret the results and seek appropriate treatment.
Assessment of Sleep Apnea Severity
Sleep apnea is classified based on the apnea-hypopnea index (AHI), which measures the number of breathing interruptions or reductions in airflow per hour of sleep. AHI scores can range from mild to severe, with mild sleep apnea having an AHI of 5-15, moderate sleep apnea having an AHI of 15-30, and severe sleep apnea having an AHI greater than 30. The severity of sleep apnea helps guide treatment decisions.

Challenges of Managing Sleep Apnea in Older Adults
Age-Related Factors
Older adults may face unique challenges in managing sleep apnea due to age-related factors. The decline in muscle tone and elasticity in the airways can contribute to airflow obstruction. Chronic medical conditions and medication use can also complicate treatment. Additionally, older adults may have a reduced capacity for coping with sleep deprivation, making it even more crucial to address sleep apnea effectively.
Coexisting Medical Conditions
Sleep apnea often occurs alongside other medical conditions commonly seen in older adults, such as obesity, hypertension, diabetes, and heart disease. These comorbidities can exacerbate the symptoms of sleep apnea and increase the risk of developing complications. Managing sleep apnea in older adults requires a comprehensive approach that addresses both the sleep disorder and underlying medical conditions.
Cognitive Impairment
Cognitive impairment can further complicate the management of sleep apnea in older adults. Sleep disturbances have been linked to cognitive decline and an increased risk of developing dementia. It is essential to prioritize the treatment of sleep apnea to improve sleep quality and potentially slow down cognitive decline in older adults.
Treatment Options for Sleep Apnea
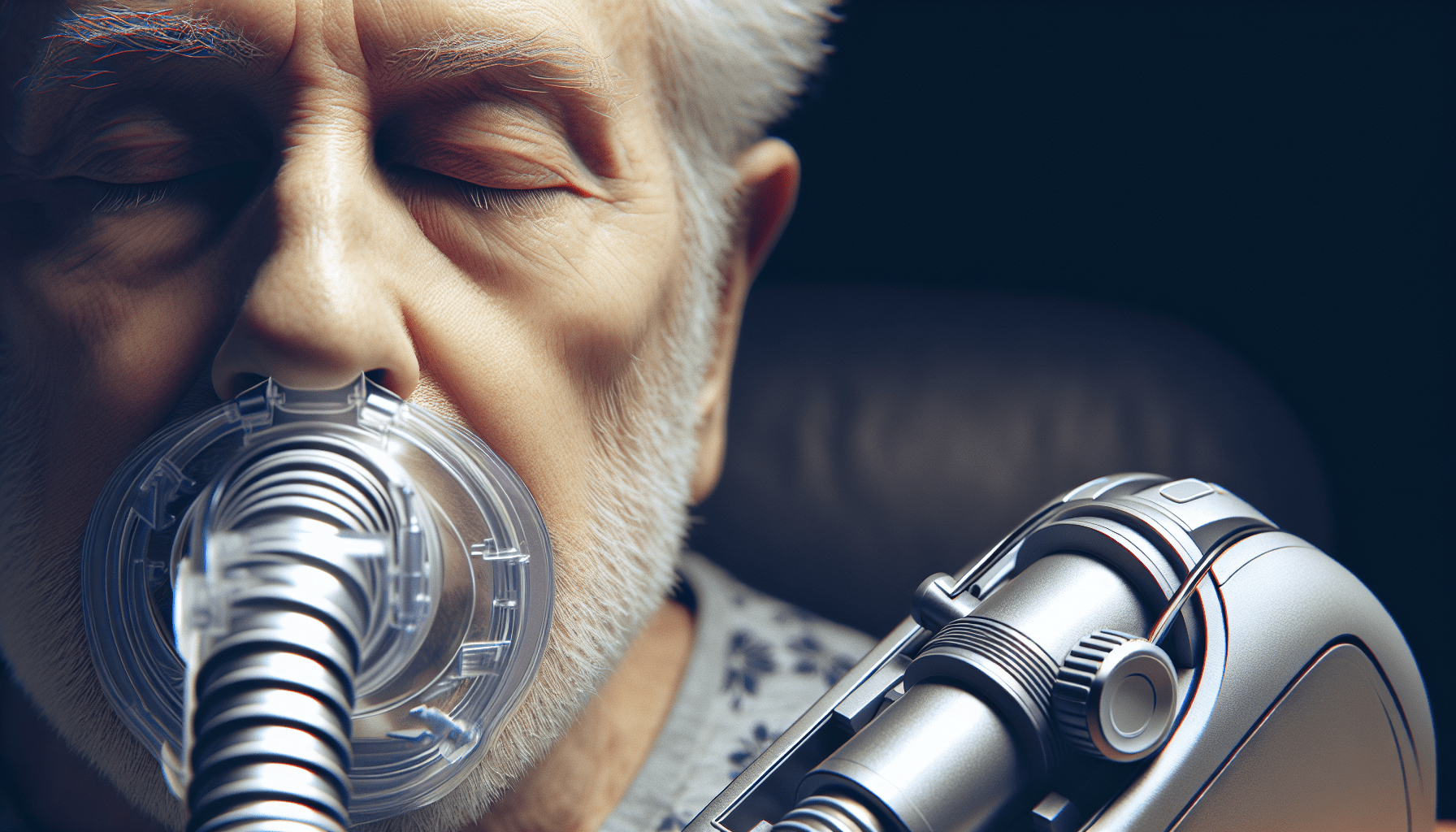
Continuous Positive Airway Pressure (CPAP)
CPAP therapy is considered the gold standard treatment for sleep apnea. It involves wearing a mask over the nose or nose and mouth during sleep, which delivers a continuous stream of air to keep the airways open. CPAP effectively reduces apnea episodes and alleviates symptoms. However, adherence to CPAP therapy can be challenging for some older adults due to discomfort, mask fit issues, and difficulty adjusting to the machine.
Oral Appliances
Oral appliances, such as mandibular advancement devices or tongue-retaining devices, can be used to treat mild to moderate obstructive sleep apnea. These devices reposition the jaw or tongue to keep the airway open during sleep. Oral appliances are a more comfortable and convenient alternative to CPAP for some older adults. However, they may not be suitable for everyone, and regular follow-up appointments with a dentist or sleep specialist are necessary.
Surgery
In some cases, surgery may be recommended to treat sleep apnea. Surgical options include uvulopalatopharyngoplasty (UPPP), which removes excess tissue from the throat, and genioglossus advancement, which repositions the tongue muscles. Surgery is usually reserved for severe cases where other treatment options have been unsuccessful or when there are specific anatomical abnormalities causing the airway obstruction.
Adherence and Compliance to Treatment
Barriers to Adherence
Adherence to sleep apnea treatment can be challenging for older adults. Common barriers include discomfort from wearing a mask or oral device, aversion to the machine noise, difficulty maintaining a consistent sleep schedule, and anxiety or claustrophobia associated with the treatment equipment. Side effects like dry mouth, nasal congestion, and skin irritation can also impact adherence.
Strategies to Improve Compliance
To improve compliance with sleep apnea treatment, it is important to address the specific barriers faced by older adults. Educating individuals about the potential benefits of treatment and providing ongoing support are crucial. Encouraging regular follow-up appointments, ensuring proper mask or oral device fit, and offering alternative treatment options can also help improve compliance. Additionally, involving caregivers or family members in the treatment process can provide additional support and motivation.
Lifestyle Modifications to Manage Sleep Apnea
Weight Loss and Exercise
Weight loss can significantly improve sleep apnea symptoms, especially in individuals with obesity. Losing excess weight reduces the amount of fatty tissue in the airways, decreasing the risk of airflow obstruction. Regular exercise also contributes to better overall health and can help alleviate sleep apnea symptoms. Engaging in physical activity, such as walking or swimming, for at least 30 minutes a day can make a positive impact.
Sleeping Position and Pillows
Changing sleeping positions can help manage sleep apnea. Sleeping on the side or in an elevated position can minimize airway obstruction. Using specialized pillows designed to promote proper head and neck alignment can also be beneficial. These pillows can help keep the airway open and prevent the tongue and soft tissues from collapsing.
Avoidance of Alcohol and Sedatives
Alcohol and sedatives can relax the muscles in the throat, increasing the risk of airway collapse during sleep. It is advisable for older adults with sleep apnea to avoid or minimize the consumption of alcohol and sedating medications, especially before bedtime. A thorough consultation with a healthcare professional is essential for evaluating medication usage and potential interactions with sleep apnea treatment.
Sleep Hygiene Practices for Better Sleep
Establishing a Consistent Sleep Schedule
Maintaining a regular sleep schedule is important for individuals with sleep apnea. Going to bed and waking up at the same time every day helps regulate the sleep-wake cycle. Creating a relaxing bedtime routine and ensuring a comfortable sleep environment can further promote better sleep.
Creating a Sleep-friendly Environment
Optimizing the sleep environment can improve sleep quality for older adults with sleep apnea. This includes keeping the bedroom quiet, dark, and cool. Using white noise machines or earplugs can help mask disruptive sounds. Investing in a comfortable mattress, pillows, and bedding can also enhance sleep comfort.
Relaxation Techniques and Mindfulness
Practicing relaxation techniques and mindfulness can help manage stress and promote better sleep. Techniques such as deep breathing exercises, progressive muscle relaxation, and guided meditation can induce a state of relaxation, making it easier to fall asleep. Incorporating these practices into the bedtime routine can have a positive impact on sleep quality.
The Role of Caregivers in Managing Sleep Apnea
Educating and Supporting Older Adults
Caregivers play a crucial role in managing sleep apnea in older adults. They can educate older adults about the importance of sleep apnea treatment, assist with equipment setup, and provide emotional support. Caregivers can also help monitor symptoms and communicate any changes to healthcare professionals.
Monitoring Adherence to Treatment
Caregivers can help ensure that older adults adhere to their sleep apnea treatment. This includes assisting with mask or oral device maintenance, troubleshooting any issues that may arise, and facilitating regular follow-up appointments. Monitoring adherence to treatment helps older adults stay on track and reap the benefits of sleep apnea management.
Improving Sleep Environment
Caregivers can create a sleep-friendly environment for older adults with sleep apnea. This involves keeping the bedroom conducive to sleep, addressing any environmental factors that may disrupt sleep, and promoting relaxation techniques or bedtime routines. By optimizing the sleep environment, caregivers can contribute to better sleep quality and overall well-being.
Prevention and Early Intervention Strategies
Screening for Sleep Apnea
Screening for sleep apnea in older adults is crucial for early detection and intervention. Healthcare professionals can use questionnaires or perform overnight pulse oximetry to identify individuals at risk of sleep apnea. Routine screenings can help prevent potential complications and improve quality of life for older adults.
Promoting Awareness and Education
Promoting awareness and education about sleep apnea is essential for prevention. By increasing knowledge about the signs and symptoms of sleep apnea, individuals and their caregivers can recognize its presence and seek appropriate medical attention. Workshops, community campaigns, and educational materials can be effective in spreading awareness.
Intervening at an Early Stage
Early intervention can significantly improve outcomes for older adults with sleep apnea. Identifying and addressing sleep apnea in its early stages can prevent the progression of symptoms and reduce the risk of developing complications. Regular check-ups and open communication with healthcare professionals are essential for timely intervention.
Improving Sleep Quality in Older Adults
Sleep Supportive Technologies
Advancements in technology have led to the development of various sleep supportive devices. These include bedside monitoring devices that track sleep patterns, wearable devices that measure sleep quality, and smart mattress systems that adjust to optimize sleep comfort. Sleep supportive technologies can help older adults monitor their sleep and make informed decisions about their sleep habits.
Sleep Education Programs
Sleep education programs tailored for older adults can provide valuable information and resources to improve sleep quality. These programs can cover topics such as sleep hygiene practices, lifestyle modifications, and the management of sleep disorders. By empowering older adults with knowledge, they can take an active role in ensuring better sleep.
Evaluating and Managing Sleep Comorbidities
Sleep apnea often coexists with other sleep disorders, such as insomnia, restless leg syndrome, or periodic limb movement disorder. These comorbidities can further disrupt sleep quality and overall well-being. It is essential to evaluate and manage any sleep-related conditions comprehensively to achieve optimal sleep for older adults.
In conclusion, understanding sleep apnea in older adults is crucial for effective management. By recognizing the types, prevalence, and causes of sleep apnea, healthcare professionals and caregivers can support older adults with appropriate diagnosis, treatment, and lifestyle modifications. Overcoming the challenges posed by age-related factors, coexisting medical conditions, and cognitive impairment requires a holistic approach that integrates various treatment options, adherence strategies, and sleep hygiene practices. With early intervention, prevention measures, and the involvement of caregivers, older adults can experience improved sleep quality and enhanced overall well-being.