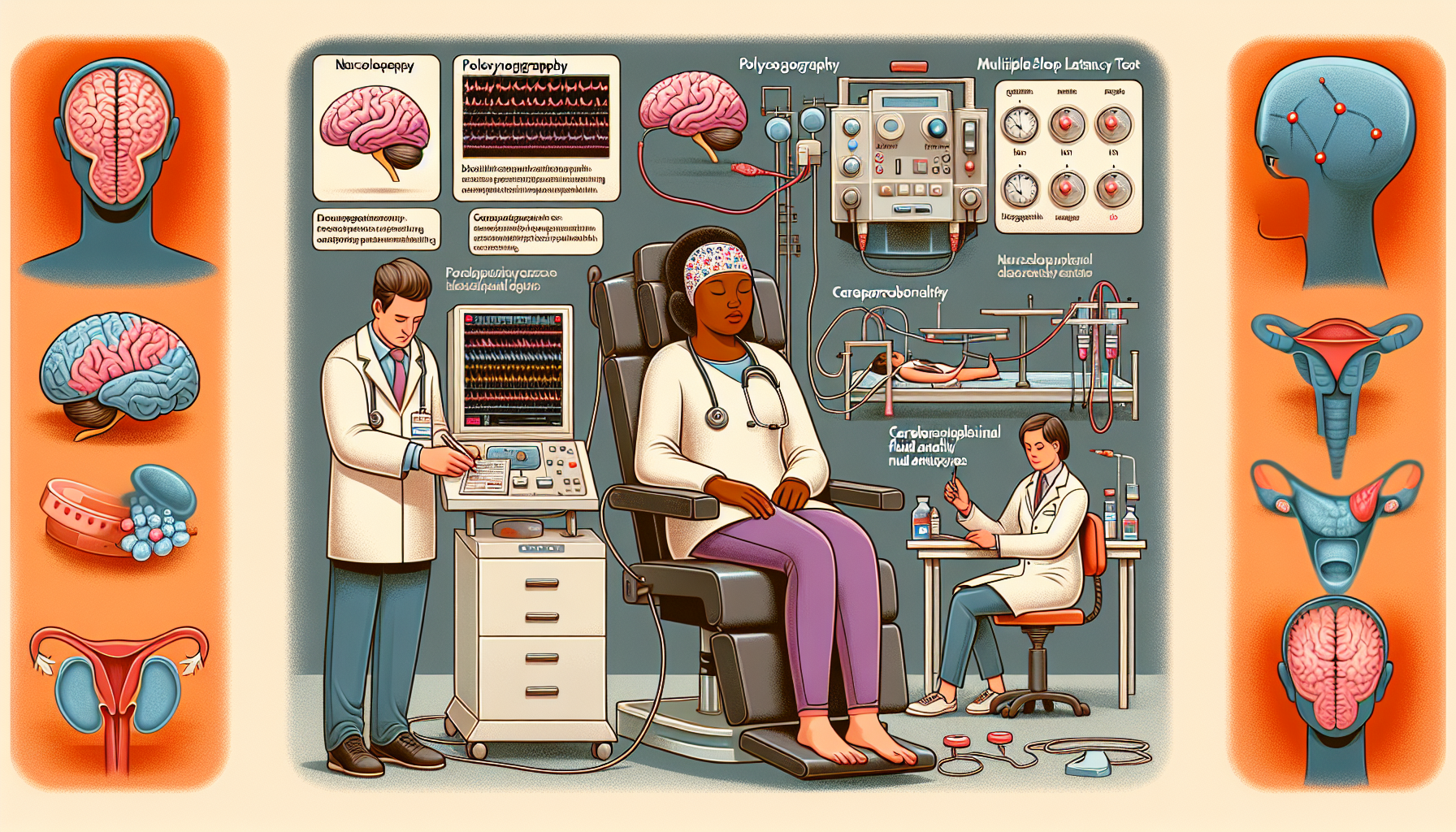
If you suspect you may have narcolepsy, it is important to understand the various tests and procedures that can help diagnose this sleep disorder. By undergoing a comprehensive evaluation, which may include a sleep study and multiple tests, you can gain a clearer understanding of your symptoms and potentially receive the appropriate treatment. In this article, we will explore the different tests and procedures used in diagnosing narcolepsy, providing you with the information you need to take the necessary steps towards better sleep and improved quality of life.
Medical History and Physical Examination
Gathering sleep-related symptoms
When diagnosing narcolepsy, gathering sleep-related symptoms is an important step. Your healthcare provider will ask you about your sleep patterns and any unusual occurrences during sleep, such as excessive daytime sleepiness, sudden loss of muscle control (cataplexy), hallucinations, or sleep paralysis. Providing detailed information about your symptoms will help in making an accurate diagnosis.
Recording medical history
Along with sleep-related symptoms, your medical history plays a vital role in diagnosing narcolepsy. Your healthcare provider will inquire about any pre-existing medical conditions, medications you are currently taking, as well as any family history of sleep disorders. It is crucial to be open and honest about your medical history to ensure an accurate diagnosis.
Conducting physical examination
A physical examination is often conducted during the diagnostic process for narcolepsy. While there are no specific physical markers for narcolepsy, the examination may help rule out other underlying conditions that could be contributing to your symptoms. Your healthcare provider will assess various aspects such as blood pressure, heart rate, and evaluate for any signs of other sleep-related disorders.
Sleep Diary and Polysomnogram
Maintaining a sleep diary
Keeping a sleep diary can provide valuable insights into your sleep patterns and help with the diagnosis of narcolepsy. You will be asked to record details such as the time you went to bed, the time you woke up, any interruptions in your sleep, and any daytime naps taken. This information will aid your healthcare provider in understanding your sleep-wake schedule and identifying any abnormalities.
Performing a polysomnogram (PSG)
A polysomnogram is a non-invasive test that measures various physiological parameters during sleep. It involves spending a night in a sleep laboratory, where electrodes are placed on your scalp, face, chest, and legs to monitor brain waves, eye movements, muscle activity, heart rate, and breathing patterns. This extensive measurement of sleep stages and associated physiological activity provides crucial information for diagnosing narcolepsy.

Multiple Sleep Latency Test (MSLT)
Purpose of the MSLT
The Multiple Sleep Latency Test (MSLT) is used to evaluate excessive daytime sleepiness and is often performed in conjunction with a polysomnogram. It measures how quickly you fall asleep in a quiet, dimly lit room during several napping opportunities throughout the day. The MSLT helps differentiate between narcolepsy and other conditions causing excessive sleepiness, such as sleep apnea or insufficient sleep.
Procedure of the MSLT
During the MSLT, you will be asked to take multiple short naps, typically every two hours, following the polysomnogram. Electrodes are attached to monitor brain waves and other physiological activity during these naps. The MSLT provides valuable information about your tendency to fall asleep and the presence of rapid eye movement (REM) sleep during the daytime, which are characteristic features of narcolepsy.
Interpreting MSLT results
An average sleep latency of less than 8 minutes and two or more instances of entering REM sleep during the MSLT are suggestive of narcolepsy. However, the test results are always interpreted in combination with your reported symptoms, medical history, and other diagnostic findings. A positive result on the MSLT may warrant further testing to confirm the diagnosis of narcolepsy.
Hypocretin-1 Testing
Analyzing cerebrospinal fluid (CSF) sample
Hypocretin-1 testing involves analyzing a sample of cerebrospinal fluid (CSF) obtained through a lumbar puncture. This test measures the levels of hypocretin-1, a neurotransmitter that regulates wakefulness and is found to be deficient in most individuals with narcolepsy with cataplexy. CSF sampling helps differentiate between type 1 narcolepsy, with low levels of hypocretin-1, and type 2 narcolepsy, which typically has normal hypocretin-1 levels.
Distinguishing between type 1 and type 2 narcolepsy
Type 1 narcolepsy, also known as narcolepsy with cataplexy, is characterized by excessive daytime sleepiness and sudden loss of muscle control triggered by strong emotions (cataplexy). This form of narcolepsy is associated with low levels of hypocretin-1. Type 2 narcolepsy, on the other hand, does not involve cataplexy and typically has normal levels of hypocretin-1. Hypocretin-1 testing helps differentiate between these two subtypes.

HLA Typing
Determining human leukocyte antigen (HLA) subtype
HLA typing is a genetic test that determines your human leukocyte antigen (HLA) subtype. HLA genes play a role in the body’s immune response. Certain HLA subtypes have been found to be more common in individuals with narcolepsy, particularly HLA-DQB1*06:02. However, HLA typing is not a diagnostic test for narcolepsy and is primarily used to support other clinical findings and aid in the diagnostic process.
Association with narcolepsy
The association between certain HLA subtypes and narcolepsy suggests a genetic susceptibility to the condition. However, it is important to note that not all individuals with the HLA-DQB1*06:02 subtype develop narcolepsy, and narcolepsy can occur in individuals without this genetic marker. HLA typing is just one aspect of the comprehensive evaluation for narcolepsy diagnosis.
Genetic Testing
Identifying potential genetic causes of narcolepsy
Genetic testing can be carried out to identify potential genetic causes of narcolepsy. Various genes have been associated with an increased risk of developing narcolepsy, including the T-cell receptor alpha locus (TCRA), the T-cell receptor beta locus (TCRB), and the purinergic receptor P2RY11. However, genetic testing is not routinely performed and is primarily reserved for research and specialized cases where there is a high suspicion of a genetic component.
Polymorphisms and variations in specific genes
Polymorphisms and variations in specific genes, such as the T-cell receptor genes and P2RY11, may increase the risk of developing narcolepsy. These variations can affect the immune system and the regulation of sleep-wake cycles. However, further research is needed to fully understand the genetic factors contributing to narcolepsy and their clinical significance in diagnosis and management.
Epworth Sleepiness Scale (ESS)
Assessing daytime sleepiness
The Epworth Sleepiness Scale (ESS) is a self-report questionnaire used to assess daytime sleepiness. It consists of eight situations in which you rate your likelihood of falling asleep on a scale from 0 to 3. The total score ranges from 0 to 24, with higher scores indicating greater daytime sleepiness. The ESS helps quantify the severity of daytime sleepiness and can be a useful tool in assessing narcolepsy symptoms.
Scoring and interpretation of ESS
Scoring for the ESS is based on the total score achieved. A score of 10 or above is generally considered indicative of excessive daytime sleepiness. However, the ESS should not be used on its own to diagnose narcolepsy, as it is not specific to this sleep disorder. It is best utilized in combination with other diagnostic measures, such as medical history, physical examination, and other objective tests.
Maintenance of Wakefulness Test (MWT)
Evaluating ability to stay awake
The Maintenance of Wakefulness Test (MWT) assesses your ability to stay awake and alert during quiet, relaxed periods. It is often performed after a polysomnogram to evaluate excessive daytime sleepiness and can be helpful in diagnosing narcolepsy. The MWT measures your ability to resist sleep and provides objective data on your wakefulness throughout the day.
Procedure and purpose of MWT
During the MWT, you are asked to sit in a quiet, darkened room and avoid any stimulating activities. Electrodes may be attached to monitor your brain waves and other physiological parameters. You will be instructed to stay awake and alert for specific periods of time, typically lasting 20-40 minutes. The MWT helps determine if you have excessive daytime sleepiness and if sleep intrusions occur during wakeful periods.
Actigraphy
Utilizing an actigraph device
Actigraphy involves wearing a small, wristwatch-like device called an actigraph to monitor your sleep-wake patterns. It is a non-invasive method that provides objective data on your sleep duration and timing. The actigraph detects movement and light exposure, which are used to estimate the periods of sleep and wakefulness. Actigraphy can provide valuable information about your sleep patterns over an extended period, aiding in the diagnosis of narcolepsy.
Monitoring sleep-wake patterns
By continuously monitoring your wrist movements and light exposure, actigraphy provides valuable information about your sleep-wake patterns. It can help identify abnormal sleep patterns, such as fragmented sleep or abnormal sleep-onset times. Actigraphy is often used in conjunction with other diagnostic tests to gather additional data on your sleep patterns and validate subjective reports of sleep disturbances.
Other Diagnostic Procedures
Psychological evaluation
A psychological evaluation may be recommended as part of the diagnostic process for narcolepsy. This evaluation aims to assess your mental health and overall psychological well-being. It may involve interviews, questionnaires, and psychological testing to rule out any psychological factors that could be contributing to your symptoms or to evaluate the impact of narcolepsy on your daily life.
Blood tests
Blood tests may be performed to evaluate various factors that can contribute to excessive sleepiness or to rule out other medical conditions. These tests can include assessing thyroid function, blood glucose levels, and vitamin D levels. Blood tests are not specific to narcolepsy but are part of the comprehensive evaluation to ensure all potential underlying causes are considered.
Electroencephalogram (EEG)
An electroencephalogram (EEG) is a test that monitors brain wave activity. It involves placing electrodes on the scalp to measure the electrical impulses generated by the brain. EEG can help identify abnormal brain wave patterns, such as those associated with narcolepsy, during wakefulness and sleep. While EEG findings alone are not diagnostic for narcolepsy, they can provide valuable information when interpreted alongside other diagnostic measures.