If you find yourself waking up tired and groggy every morning, struggling to stay focused throughout the day, you might be one of the millions of people living with sleep apnea. This common sleep disorder is characterized by pauses in breathing during sleep, which can lead to numerous health issues if left untreated. In this article, we will explore the diagnosis of sleep apnea, shedding light on the various tests and examinations that healthcare professionals use to identify this condition accurately. So, let’s embark on this informative journey together and gain a better understanding of sleep apnea and its diagnostic procedures.
Overview of Sleep Apnea
Sleep apnea is a sleep disorder characterized by pauses in breathing or instances of shallow or infrequent breathing during sleep. These breathing pauses can last anywhere from a few seconds to minutes and can occur multiple times throughout the night. As a result, the quality of sleep is severely disrupted, leading to a range of symptoms and health complications. Sleep apnea affects both adults and children, although it is more commonly seen in adults. Understanding the definition, types, and prevalence of sleep apnea is crucial in recognizing and managing this condition effectively.
Definition of sleep apnea
Sleep apnea is defined as a sleep disorder in which the individual experiences pauses in breathing or shallow breathing during sleep. These episodes, known as apneas, can be obstructive, central, or a combination of both. Obstructive sleep apnea (OSA) is the most common form, occurring when the airway is partially or completely blocked during sleep, usually due to relaxed throat muscles. Central sleep apnea (CSA) is less common and involves the brain failing to signal the muscles to breathe. Mixed sleep apnea is a combination of obstructive and central sleep apnea.
Types of sleep apnea
As mentioned earlier, sleep apnea can be categorized into three main types: obstructive sleep apnea (OSA), central sleep apnea (CSA), and mixed sleep apnea. Obstructive sleep apnea occurs due to a physical blockage or collapse of the airway during sleep, leading to pauses in breathing. Central sleep apnea is caused by a failure of the brain to send the appropriate signals to the muscles that control breathing. Mixed sleep apnea is a combination of both obstructive and central sleep apnea.
Prevalence of sleep apnea
Sleep apnea is a highly prevalent sleep disorder, affecting millions of people worldwide. It is estimated that approximately 26% of adults between the ages of 30 and 70 have sleep apnea. However, many cases of sleep apnea go undiagnosed, making it challenging to determine the true prevalence. Men are more commonly affected by sleep apnea than women, although the risk increases in women after menopause. The prevalence of sleep apnea also increases with age and weight gain. It is important to note that sleep apnea can affect individuals of any age, including children, although it is less prevalent in this population.
Signs and Symptoms
Recognizing the signs and symptoms of sleep apnea is crucial in identifying and seeking proper diagnosis and treatment. While not everyone with sleep apnea experiences the same symptoms, the following are common indicators of the condition:
Loud snoring
One of the most common symptoms of sleep apnea is loud, disruptive snoring. This snoring is usually more prominent during obstructive apneas when the airway is partially or fully blocked. The snoring may be so loud that it disturbs the sleep of others in the household.
Episodes of breathing cessation during sleep
Individuals with sleep apnea experience pauses in breathing during sleep. These pauses, often noticed by a partner or family member, can last for a few seconds to a minute and are often followed by a snort or gasp as breathing resumes. These episodes disrupt the sleep cycle and can occur multiple times throughout the night.
Excessive daytime sleepiness
Daytime sleepiness is a hallmark symptom of sleep apnea. Despite spending what seems like a full night’s sleep in bed, individuals with sleep apnea often wake up feeling unrested and excessively tired throughout the day. This excessive sleepiness can interfere with daily activities and increase the risk of accidents, such as falling asleep while driving.
Morning headaches
Waking up with a headache, especially in the morning, is a common symptom of sleep apnea. These headaches are often due to the decreased oxygen levels and increased carbon dioxide levels that occur during apneas.
Irritability and mood changes
The disrupted sleep caused by sleep apnea can have a significant impact on an individual’s mood and overall well-being. Those with sleep apnea often experience irritability, mood swings, and feelings of depression or anxiety.
Difficulty concentrating
Sleep apnea can impair cognitive function and make it challenging to concentrate, focus, and remember information. This can affect work, school, and daily activities, leading to reduced productivity and performance.
Memory problems
Sleep apnea has been linked to memory problems, particularly with regards to short-term memory. Individuals may find it difficult to recall details or events that occurred recently.
Restless sleep
Sleep apnea disrupts the normal sleep patterns, leading to restless sleep. Individuals with sleep apnea may constantly shift positions, toss and turn, and regularly wake up during the night.
Waking up with a dry mouth or sore throat
Breathing through the mouth during sleep can cause dry mouth and a sore throat upon waking. This occurs when the airway becomes blocked or the individual resorts to mouth breathing due to blocked nasal passages.

Risk Factors and Causes
Understanding the risk factors and causes of sleep apnea can help identify individuals who may be at a higher risk of developing the condition. While anyone can develop sleep apnea, certain factors increase the likelihood of its occurrence:
Obesity and excess weight
One of the most significant risk factors for sleep apnea is having excess body weight or obesity. The excess fat in the neck area can obstruct the airway, increasing the risk of apneas during sleep.
Age (middle-aged or older adults)
As individuals age, the risk of developing sleep apnea increases. The muscles in the throat naturally become weaker, making it more likely for the airway to collapse during sleep.
Sex (males are more prone to sleep apnea)
Men are more commonly affected by sleep apnea than women. However, women’s risk of developing sleep apnea increases after menopause.
Family history
Sleep apnea can run in families, suggesting a genetic component to the condition. Having a close family member with sleep apnea increases the risk of developing the disorder.
Lifestyle factors (smoking, alcohol, sedatives)
Engaging in certain lifestyle habits, such as smoking, consuming alcohol, or taking sedatives, can increase the risk of sleep apnea. These substances can relax the muscles and interfere with breathing during sleep.
Nasal congestion and abnormalities
Nasal congestion, whether from allergies or structural abnormalities, can obstruct airflow and contribute to sleep apnea. Conditions such as a deviated septum or chronic sinus problems can increase the risk.
Medical conditions (hypertension, heart disorders, diabetes)
Certain medical conditions are associated with an increased risk of sleep apnea. Hypertension (high blood pressure), heart disorders, and diabetes are examples of conditions that can contribute to the development of sleep apnea.
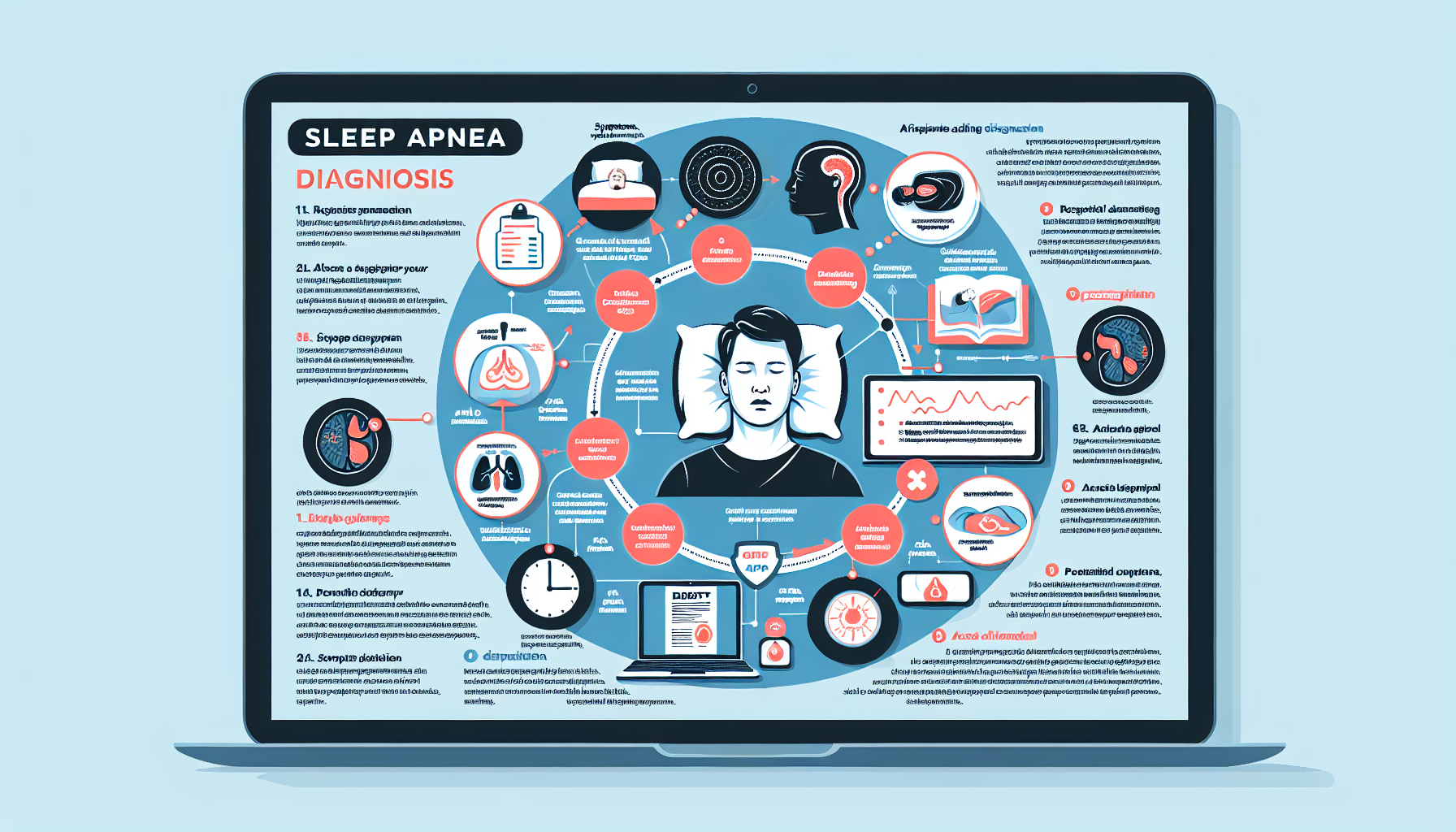
Diagnostic Methods
Properly diagnosing sleep apnea is essential in order to develop an effective treatment plan. Several diagnostic methods may be utilized to determine the presence and severity of sleep apnea:
Medical history and symptom assessment
A healthcare professional will typically start with a thorough medical history and symptom assessment. This involves discussing the individual’s sleep patterns, snoring habits, and notable symptoms. Additionally, factors such as family history, medications, and lifestyle habits will be evaluated.
Physical examination
A physical examination may be conducted to assess the individual’s overall health and identify any physical factors that may contribute to sleep apnea. Examination of the throat, neck, and oral cavity can provide valuable information.
Sleep study (polysomnography)
The gold standard for diagnosing sleep apnea is a sleep study, also known as polysomnography. This overnight test is typically done at a sleep center or hospital. It involves monitoring various physiological parameters during sleep, such as brain activity, eye movements, muscle activity, heart rate, and breathing patterns. This allows healthcare professionals to assess the occurrence and severity of apneas and other sleep-related disorders.
Home sleep apnea testing
In some cases, a healthcare professional may recommend a home sleep apnea test as an alternative to a sleep center study. This involves the individual wearing portable monitoring devices while sleeping in the comfort of their own bed. The data collected can provide valuable insights into the presence of sleep apnea.
Oximetry measurement
Oximetry measurement involves using a pulse oximeter to monitor oxygen levels in the blood during sleep. While not as comprehensive as a sleep study, oximetry can help determine if oxygen levels drop significantly during apneas or other breathing abnormalities.
Epworth Sleepiness Scale
The Epworth Sleepiness Scale is a simple questionnaire that assesses an individual’s tendency to fall asleep during daily activities, providing a measure of daytime sleepiness. This scale is often used as a part of the diagnostic process to evaluate the severity of sleep apnea symptoms.

Medical Professionals Involved in Diagnosis
Diagnosing sleep apnea often involves a team of medical professionals with expertise in sleep medicine and related fields. The following healthcare professionals commonly play a role in the diagnosis of sleep apnea:
Primary care physician
A primary care physician is often the first point of contact for individuals seeking evaluation of their symptoms. They can assess symptoms, evaluate risk factors, and refer patients to specialists for further evaluation if necessary.
Sleep medicine specialist
A sleep medicine specialist is a physician with expertise in the diagnosis and treatment of sleep disorders, including sleep apnea. They play a crucial role in analyzing sleep study results, interpreting diagnostic tests, and developing treatment plans.
Otolaryngologist
An otolaryngologist, also known as an ear, nose, and throat (ENT) specialist, may be involved in the diagnosis of sleep apnea. They can evaluate the upper airway for any structural abnormalities or obstructions that may contribute to sleep apnea.
Pulmonologist
A pulmonologist is a physician who specializes in the diagnosis and treatment of lung and respiratory disorders. They are often involved in the evaluation and management of sleep apnea, particularly in cases where the disorder is associated with underlying lung conditions.
Neurologist
A neurologist is a medical professional who specializes in the diagnosis and treatment of disorders of the nervous system. In some cases, they may be consulted to evaluate any neurological factors that may contribute to sleep apnea or its associated symptoms.
Dentist
Dentists who have specialized training in dental sleep medicine may also be involved in the diagnosis of sleep apnea. They can assess the structure and position of the jaw, tongue, and soft tissues of the mouth, which can impact airway patency during sleep.
Screening and Questionnaires
Screening for sleep apnea often involves the use of validated questionnaires to assess the likelihood of the condition. These questionnaires can help identify individuals who may benefit from further evaluation:
STOP-BANG questionnaire
The STOP-BANG questionnaire is a widely used screening tool for sleep apnea. It assesses snoring habits, daytime sleepiness, and other risk factors for sleep apnea. The questionnaire includes questions related to body mass index (BMI), age, gender, and neck circumference.
Berlin Questionnaire
The Berlin Questionnaire is another commonly used tool for screening sleep apnea. It consists of questions related to snoring habits, daytime sleepiness, and the presence of high blood pressure. The questionnaire categorizes individuals into low, intermediate, or high risk for sleep apnea.
STOP questionnaire
Similar to the STOP-BANG questionnaire, the STOP questionnaire assesses snoring habits, daytime sleepiness, tiredness, observed apneas, and blood pressure. It is a relatively simple tool that can be used as a preliminary screening tool.
Epworth Sleepiness Scale
As mentioned earlier, the Epworth Sleepiness Scale is used to assess an individual’s propensity to fall asleep during daily activities. It can help gauge the severity of excessive daytime sleepiness and its impact on daily functioning.
American Academy of Sleep Medicine (AASM) criteria
The American Academy of Sleep Medicine (AASM) has established criteria for diagnosing sleep apnea, taking into consideration clinical symptoms, severity of symptoms, and diagnostic test results. These criteria serve as a guideline for healthcare professionals in determining the presence and severity of sleep apnea.
Sleep Apnea Severity Assessment
Assessing the severity of sleep apnea is essential in determining the most appropriate treatment approach. Several parameters and indices are used to gauge the severity of sleep apnea:
Apnea-Hypopnea Index (AHI)
The Apnea-Hypopnea Index (AHI) is a measure used to quantify the number of apneas and hypopneas that occur per hour of sleep. It is calculated by dividing the total number of apneas and hypopneas by the total number of hours slept.
Oxygen Desaturation Index (ODI)
The Oxygen Desaturation Index (ODI) measures the number of times per hour that blood oxygen levels drop below a certain threshold during apneas and hypopneas. This index provides insight into the impact of sleep apnea on blood oxygenation.
Respiratory Disturbance Index (RDI)
The Respiratory Disturbance Index (RDI) is similar to the AHI, but it includes additional respiratory events such as respiratory effort-related arousals (RERAs). The RDI provides a comprehensive measure of respiratory disturbances during sleep.
Scoring of sleep stages and arousals
Sleep studies also involve scoring sleep stages and arousals. This information is crucial in understanding the impact of sleep apnea on the overall sleep architecture. It can help identify any disruptions in normal sleep patterns and assess the quality of sleep.
Classification of sleep apnea severity
Based on the AHI, sleep apnea can be classified into four severity categories: mild, moderate, severe, and very severe. The severity classification helps guide treatment decisions and provides a framework for understanding the impact of sleep apnea on an individual’s health.
Additional Testing and Evaluation
In some cases, additional tests and evaluations may be necessary to assess the impact of sleep apnea on overall health and identify any related complications:
Blood tests
Blood tests may be conducted to assess various parameters related to overall health and evaluate for conditions that may be associated with sleep apnea, such as thyroid disorders, diabetes, or hormonal imbalances.
Imaging studies (X-ray, CT scan, MRI)
Imaging studies, such as X-rays, CT scans, or MRIs, of the head, neck, and upper airway may be performed to evaluate for obstructions or abnormalities that may contribute to sleep apnea.
Electrocardiogram (ECG)
An electrocardiogram (ECG) is a non-invasive test that records the electrical activity of the heart. It can be used to assess the impact of sleep apnea on cardiovascular health and identify any underlying cardiac conditions.
Echocardiogram
An echocardiogram uses ultrasound waves to create images of the heart. This test can help evaluate heart structure and function, providing valuable insights into the impact of sleep apnea on cardiac health.
Pulmonary function tests
Pulmonary function tests assess lung function and can help identify any underlying respiratory conditions or abnormalities that may contribute to sleep apnea.
Differential Diagnosis
While sleep apnea is a commonly diagnosed sleep disorder, it is essential to rule out other potential causes of the symptoms. The following conditions may present similar symptoms and should be considered in the differential diagnosis:
Other sleep disorders (narcolepsy, circadian rhythm disorders)
Other sleep disorders, such as narcolepsy or circadian rhythm disorders, can cause excessive daytime sleepiness and disrupted sleep patterns. These conditions may need to be evaluated to ensure an accurate diagnosis.
Upper airway resistance syndrome
Upper airway resistance syndrome (UARS) is a condition characterized by increased resistance in the upper airway during sleep, causing snoring, increased effort to breathe, and sleep disruption. UARS can be a precursor to the development of sleep apnea.
Obesity hypoventilation syndrome
Obesity hypoventilation syndrome (OHS) is a condition in which individuals who are obese experience reduced ventilation, leading to low levels of oxygen and high levels of carbon dioxide in the blood. OHS is often associated with sleep apnea but requires specific diagnostic criteria for its diagnosis.
Chronic fatigue syndrome
Chronic fatigue syndrome (CFS) is a complex condition characterized by persistent fatigue that is not relieved by rest and is not directly caused by other medical or psychiatric conditions. While fatigue is a symptom common to both sleep apnea and CFS, a thorough evaluation is necessary to differentiate between the two.
Depression
Depression can often cause sleep disturbances, including disrupted sleep patterns and excessive daytime sleepiness. Identifying and evaluating for depression is crucial in determining the appropriate treatment approach.
Anxiety disorders
Anxiety disorders, such as generalized anxiety disorder or panic disorder, can also cause sleep disturbances and symptoms similar to sleep apnea. A comprehensive evaluation is necessary to differentiate between anxiety-related sleep disturbances and sleep apnea.
Thyroid disorders
Thyroid disorders, particularly hypothyroidism, can contribute to sleep disturbances and excessive daytime sleepiness. Assessing thyroid function is necessary to rule out any underlying thyroid-related causes of the symptoms.
Conclusion
Sleep apnea is a common and potentially serious sleep disorder that can significantly impact an individual’s quality of life. It is important to recognize the signs and symptoms of sleep apnea and seek a proper diagnosis from qualified healthcare professionals. Understanding the risk factors for sleep apnea and the different diagnostic methods available can facilitate early detection and appropriate treatment. With proper management, individuals with sleep apnea can experience improved sleep quality, reduced symptoms, and overall better health and well-being.