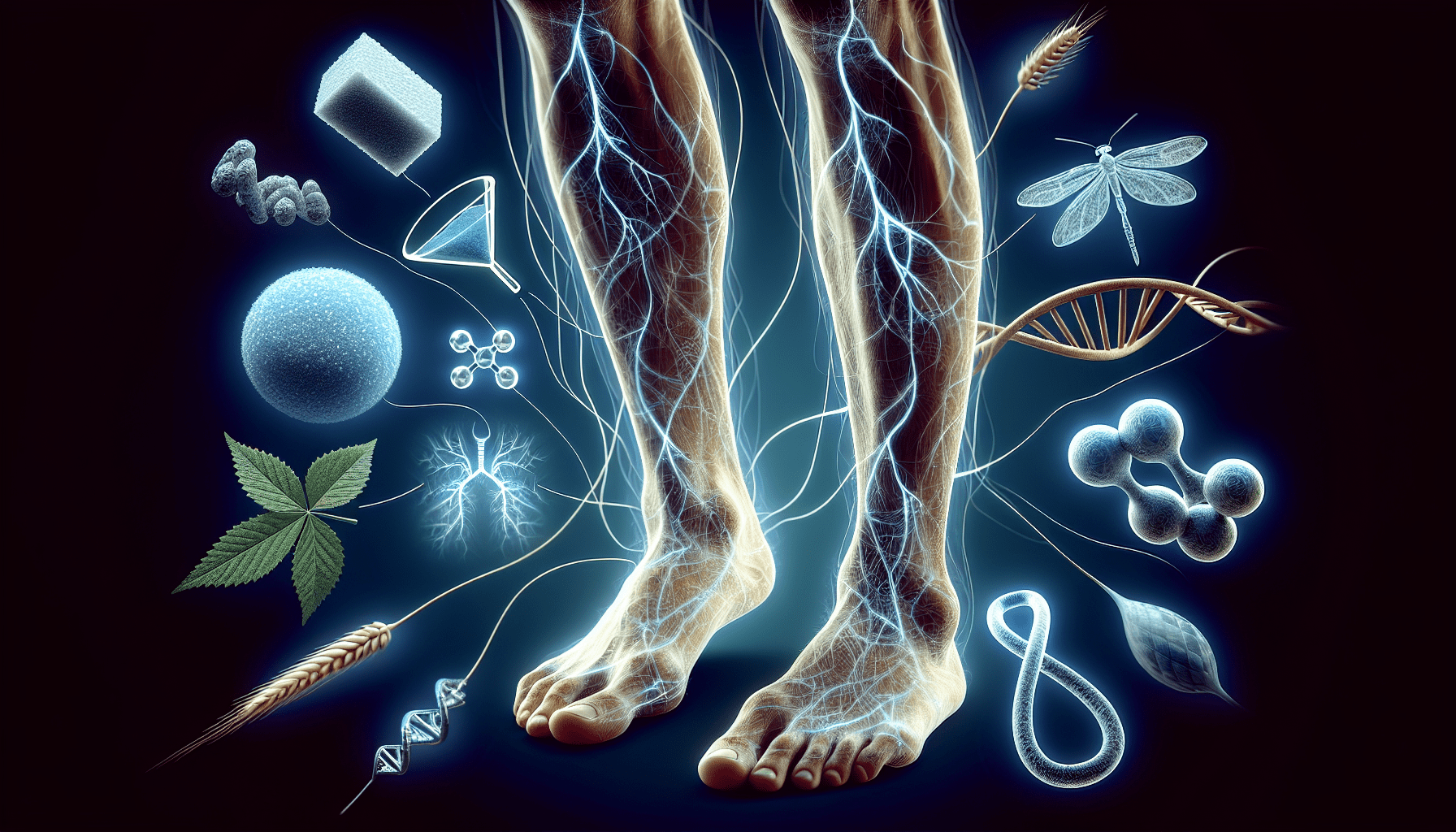
If you’ve ever experienced the uncontrollable urge to twitch your legs while trying to sleep, you may be familiar with Restless Legs Syndrome (RLS). But did you know that this seemingly harmless condition could be linked to chronic illnesses? Recent studies have shed light on a surprising connection between RLS and conditions such as cardiovascular disease, diabetes, and mental health disorders. In this article, we will explore the intriguing relationship between Restless Legs Syndrome and chronic illnesses, uncovering the potential implications and offering insights into managing both. So, get ready to unlock the mystery behind those restless legs and discover how they may be connected to your overall well-being.

What is Restless Legs Syndrome (RLS)?
Restless Legs Syndrome (RLS) is a neurological disorder characterized by an uncontrollable urge to move one’s legs, often accompanied by uncomfortable sensations. While the exact cause of RLS is still unknown, it is believed to be related to abnormalities in the brain’s dopamine system. The symptoms of RLS typically worsen during periods of rest or inactivity, making it difficult for individuals to relax and fall asleep. RLS can have a significant impact on a person’s quality of life, affecting their sleep, mood, and overall well-being.
Definition of RLS
Restless Legs Syndrome is defined as a condition where individuals experience an overwhelming need to move their legs due to uncomfortable sensations. These sensations are often described as aching, itching, tingling, or crawling, and can range from mild to severe in intensity. The urge to move the legs can be temporarily relieved by movement, but the relief is usually only temporary. RLS symptoms typically occur or worsen during the evening or at night, leading to difficulty falling asleep and staying asleep.
Common symptoms of RLS
The most common symptom of RLS is an irresistible urge to move the legs, usually accompanied by uncomfortable and distressing sensations. These sensations are often described as creeping, crawling, burning, or tingling, and can sometimes be painful. The intensity of these sensations can vary from person to person and can range from mild to severe. In addition to the physical discomfort, RLS can also cause sleep disturbances, leading to excessive daytime sleepiness and fatigue.
Prevalence of RLS
Restless Legs Syndrome is more common than previously thought, with studies estimating that it affects up to 10% of the population worldwide. The prevalence of RLS increases with age, with older adults being more likely to experience symptoms. It is also more common in women than in men. While RLS can occur at any age, it often starts in middle-aged or elderly individuals. RLS can have a significant impact on a person’s quality of life, interfering with their ability to perform daily activities and affecting their overall well-being.
Overview of Chronic Illnesses
Chronic illnesses are long-term medical conditions that generally cannot be cured but can only be managed. These conditions often require ongoing medical care and can have a significant impact on a person’s physical, emotional, and social well-being. Examples of chronic illnesses include heart disease, diabetes, asthma, arthritis, and chronic pain conditions. While the specific symptoms and challenges can vary depending on the condition, chronic illnesses often share similar characteristics and require comprehensive management strategies.
Types and examples of chronic illnesses
Chronic illnesses encompass a wide range of medical conditions that can affect different parts of the body and systems. Some common types of chronic illnesses include cardiovascular diseases such as hypertension and coronary artery disease, neurological disorders such as multiple sclerosis and Parkinson’s disease, psychiatric conditions such as depression and anxiety disorders, autoimmune disorders such as rheumatoid arthritis and lupus, metabolic disorders such as diabetes and obesity, and kidney diseases such as chronic kidney disease and end-stage renal disease.
Common symptoms and challenges of chronic illnesses
Chronic illnesses can cause a variety of symptoms that can significantly impact a person’s daily life. These symptoms can include pain, fatigue, difficulty breathing, cognitive impairment, mood disturbances, sleep disturbances, and physical limitations. Managing these symptoms and the related challenges can be a constant struggle for individuals living with chronic illnesses. Additionally, chronic illnesses often require complex and long-term treatments, frequent medical appointments, and lifestyle modifications, which can further contribute to the burden of these conditions.
Prevalence and impact of chronic illnesses
Chronic illnesses have become a significant public health concern, affecting millions of people worldwide. According to the World Health Organization, chronic diseases are the leading cause of death and disability globally, with approximately 70% of deaths worldwide attributed to chronic conditions. The prevalence of chronic illnesses is expected to continue rising due to factors such as aging populations, unhealthy lifestyles, and environmental factors. The impact of chronic illnesses extends beyond the individual level, affecting families, communities, and healthcare systems. Addressing the complex challenges posed by chronic illnesses requires a comprehensive and multidisciplinary approach.
Research and Studies on RLS and Chronic Illnesses
Research studies have explored the link between Restless Legs Syndrome and chronic illnesses, shedding light on the potential associations and mechanisms underlying these conditions.
Findings from medical research
Numerous studies have examined the relationship between RLS and various chronic illnesses, revealing intriguing connections. For example, research has shown a higher prevalence of RLS among individuals with cardiovascular diseases, neurological disorders, psychiatric conditions, autoimmune disorders, metabolic disorders, and kidney diseases. Furthermore, some studies have indicated that the presence of RLS may worsen the symptoms and prognosis of these comorbid conditions. The research findings provide valuable insights into the complex interplay between RLS and chronic illnesses.
Association between RLS and specific chronic illnesses
Studies have demonstrated a bidirectional relationship between RLS and chronic illnesses. Individuals with chronic illnesses have a higher likelihood of experiencing RLS symptoms, and conversely, individuals with RLS are more likely to develop certain chronic conditions. This association suggests that RLS may serve as both a consequence and a risk factor for the development and progression of chronic illnesses. Understanding these associations can help inform diagnosis, treatment, and management strategies for individuals affected by both RLS and chronic illnesses.
Mechanisms and theories linking RLS to chronic illnesses
Scientists and researchers have proposed several theories and mechanisms to explain the possible connections between RLS and chronic illnesses. One theory suggests that shared genetic factors and biological pathways may contribute to the development of both RLS and certain chronic conditions. Another theory proposes that inflammation and dysregulation of the immune system may play a role in the development and progression of both RLS and chronic illnesses. Additionally, studies have found abnormalities in dopamine and iron regulation in individuals with RLS, which may be implicated in the pathophysiology of both RLS and some chronic illnesses. Sleep disturbances, which are commonly experienced by individuals with RLS, may also contribute to the development or exacerbation of chronic illnesses.
Chronic Illnesses Associated with RLS
Restless Legs Syndrome has been found to be associated with various chronic illnesses across different medical specialties.
Cardiovascular diseases
There is evidence to suggest a significant association between RLS and cardiovascular diseases such as hypertension, coronary artery disease, and stroke. Individuals with RLS may have an increased risk of developing cardiovascular diseases, and the presence of RLS may negatively impact the prognosis and management of these conditions. Further research is needed to elucidate the underlying mechanisms linking RLS and cardiovascular diseases and to explore potential treatment strategies.
Neurological disorders
Restless Legs Syndrome has been found to be more common in individuals with neurological disorders such as Parkinson’s disease, multiple sclerosis, and peripheral neuropathy. These conditions share similar neurobiological pathways with RLS, suggesting a potential connection. Managing RLS symptoms in individuals with neurological disorders can be particularly challenging due to overlapping symptoms and treatment considerations.
Psychiatric conditions
The association between RLS and psychiatric conditions, including depression and anxiety disorders, has been well-documented. Studies have shown that individuals with psychiatric conditions are more likely to experience RLS symptoms, and the presence of RLS can exacerbate psychiatric symptoms. The bidirectional relationship between RLS and psychiatric conditions highlights the need for a holistic approach to the management of these comorbidities.
Autoimmune disorders
Chronic autoimmune disorders such as rheumatoid arthritis and systemic lupus erythematosus have been associated with an increased risk of developing RLS. The underlying inflammatory processes in these conditions may contribute to the development or worsening of RLS symptoms. Effective management of both RLS and autoimmune disorders requires a comprehensive treatment plan addressing the specific needs of each individual.
Metabolic disorders
Restless Legs Syndrome has also been linked to metabolic disorders such as diabetes and obesity. The relationship between RLS and metabolic disorders is complex and multifaceted, involving shared genetic factors, common comorbidities, and potential metabolic dysregulation. Managing RLS symptoms in individuals with metabolic disorders can be challenging, as certain medications used to control these conditions may worsen RLS symptoms.
Kidney diseases
Studies have shown a higher prevalence of RLS in individuals with chronic kidney disease and end-stage renal disease. The exact mechanisms underlying this association are not yet fully understood, but factors such as iron deficiency, uremic toxins, and altered dopamine regulation may play a role. The presence of RLS in individuals with kidney diseases can further compound the already significant burden of these conditions.
Shared Risk Factors and Biological Pathways
Several shared risk factors and biological pathways have been identified that may contribute to the development and progression of both RLS and chronic illnesses.
Genetic factors
Genetic factors appear to play a role in both RLS and various chronic illnesses. Certain gene variants have been associated with an increased risk of developing RLS, as well as specific chronic conditions. Shared genetic factors may help explain the association between RLS and chronic illnesses and provide insights into potential underlying mechanisms.
Inflammation and immune system involvement
Inflammation and dysregulation of the immune system have been implicated in the pathogenesis of both RLS and chronic illnesses. Chronic inflammation can disrupt normal biological processes and contribute to the development and progression of various medical conditions. Inflammatory markers have been found to be elevated in individuals with RLS as well as in those with chronic illnesses, suggesting a possible link.
Dopamine and iron dysregulation
Abnormalities in dopamine and iron regulation have been observed in individuals with RLS and certain chronic diseases. Dopamine is a neurotransmitter involved in the regulation of movement, reward, and mood. Iron is essential for the production and transport of dopamine in the brain. Disruptions in dopamine and iron homeostasis may contribute to the development of both RLS and chronic illnesses. Medications that affect dopamine or iron levels may be used in the treatment of RLS and certain chronic conditions.
Sleep disturbances
Sleep disturbances are a common feature of both RLS and many chronic illnesses. Disrupted sleep patterns can lead to a variety of health problems, exacerbating the symptoms and burden of chronic conditions. Improving sleep quality and addressing underlying sleep disturbances may have a positive impact on both RLS and chronic illnesses.
Impact of RLS on Chronic Illnesses
The presence of RLS in individuals with chronic illnesses can have significant implications for symptom management, quality of life, and treatment outcomes.
Exacerbation of symptoms and quality of life
RLS can exacerbate the symptoms and burden of chronic illnesses. Sleep disturbances caused by RLS can lead to increased fatigue, decreased cognitive function, and worsened mood, all of which can further impair a person’s quality of life. The discomfort and distress associated with RLS symptoms can also interfere with the management of chronic conditions, making it challenging for individuals to adhere to treatment plans and engage in self-care activities.
Management challenges
Managing RLS symptoms in individuals with chronic illnesses can be complex and challenging. The presence of multiple comorbidities may require careful consideration of potential drug interactions and treatment strategies. Additionally, some medications used to manage chronic illnesses may worsen RLS symptoms or interact with RLS medications. A comprehensive and individualized approach to management is crucial to address the unique needs and challenges faced by individuals with both RLS and chronic illnesses.
Treatment considerations for patients with both RLS and chronic illnesses
When treating individuals with both RLS and chronic illnesses, healthcare professionals must consider the potential interactions and side effects of medications used to manage both conditions. Communication and coordination between healthcare providers involved in the treatment of the various conditions are essential to ensure the best possible outcomes. Non-pharmacological interventions, such as lifestyle modifications and relaxation techniques, may also play a role in managing RLS symptoms and improving overall well-being.
Management Approaches for RLS and Chronic Illnesses
Various treatment options and strategies are available for managing both RLS and chronic illnesses, offering hope for improved symptom control and quality of life.
Medications and therapies for RLS
Several classes of medications have been approved for the treatment of RLS. These include dopamine agonists, opioid medications, anticonvulsants, and benzodiazepines. Medication selection and dosage should be tailored to each individual’s specific needs and medical history. In addition to medications, non-pharmacological approaches such as exercise, massage, heat or cold therapy, and relaxation techniques may provide relief from RLS symptoms.
Treatment strategies for chronic illnesses
The management of chronic illnesses often involves a combination of lifestyle modifications, medications, and supportive therapies. Treatment strategies are typically tailored to each individual’s specific condition and may include physical activity, diet modifications, medication regimens, rehabilitation programs, and mental health support. Regular monitoring and follow-up care are important to ensure treatment effectiveness and make adjustments as necessary.
Multidisciplinary and holistic approaches
Given the complexity and impact of both RLS and chronic illnesses, a multidisciplinary and holistic approach to management is often necessary. This may involve a team of healthcare professionals, including primary care physicians, specialists, nurses, pharmacists, physical therapists, and mental health professionals. Collaborative care can help address the diverse needs and challenges faced by individuals with both RLS and chronic illnesses, improving symptom control, treatment outcomes, and overall well-being.
Improving Awareness and Diagnosis
Enhancing awareness and promoting early diagnosis of RLS in individuals with chronic illnesses is essential for optimal management and improved quality of life.
Recognizing RLS symptoms in patients with chronic illnesses
Healthcare providers should be vigilant in recognizing the symptoms of RLS in individuals with chronic illnesses. Recognizing the unique characteristics of RLS, such as the urge to move the legs and the uncomfortable sensations, can help differentiate it from other conditions and facilitate appropriate diagnosis and treatment.
Importance of early detection and intervention
Early detection and intervention in RLS can lead to better symptom control and management of chronic illnesses. Identifying RLS in individuals with chronic illnesses can help tailor treatment plans to target both conditions simultaneously, improving overall outcomes and well-being.
Role of healthcare professionals
Healthcare professionals play a vital role in raising awareness about the association between RLS and chronic illnesses. They can educate individuals with chronic illnesses about RLS symptoms, risk factors, and potential treatment options. Healthcare professionals can also advocate for interdisciplinary collaboration and the development of comprehensive management strategies to address the complex needs of individuals with both RLS and chronic illnesses.
Impact of Treating RLS on Chronic Illnesses
Treating RLS in individuals with chronic illnesses can potentially have positive effects on the management of the comorbid conditions.
Potential improvements in chronic illness symptoms
Effective management of RLS symptoms, including the relief of discomfort and improvement in sleep quality, may result in reduced symptom severity and improved overall well-being in individuals with chronic illnesses. By addressing RLS as part of the comprehensive treatment plan, healthcare professionals can potentially enhance the management of chronic conditions and improve treatment outcomes.
Effectiveness of RLS treatment on comorbid conditions
Studies have shown that treating RLS in individuals with chronic illnesses can lead to improvements in the symptoms and management of the comorbid conditions. For example, controlling RLS symptoms in individuals with cardiovascular diseases may contribute to better blood pressure control and cardiovascular outcomes. Similarly, addressing RLS in individuals with psychiatric conditions may help alleviate psychiatric symptoms and improve overall mental health.
Enhancing overall patient well-being
By effectively managing RLS symptoms, healthcare professionals can enhance the overall well-being and quality of life of individuals with chronic illnesses. Improving sleep quality, reducing discomfort, and alleviating fatigue can positively impact a person’s physical, emotional, and social functioning, leading to a better overall quality of life.
Future Directions for Research and Management
The field of RLS and chronic illnesses continues to evolve, offering exciting possibilities for future research and management approaches.
Exploring novel treatment options
Ongoing research is focused on identifying novel treatment options for both RLS and chronic illnesses. The development of targeted therapies that address the underlying mechanisms and pathophysiology of RLS and specific chronic conditions may offer new hope for improved symptom control and better treatment outcomes.
Long-term outcomes and follow-up studies
Long-term outcomes of individuals with both RLS and chronic illnesses are an area of interest for future research. Understanding the long-term impact of RLS on the progression and prognosis of chronic conditions can help guide treatment decisions and improve patient care.
Interdisciplinary collaborations
Further interdisciplinary collaborations are needed to advance the field of RLS in the context of chronic illnesses. Collaboration among researchers, healthcare providers, and patient advocacy groups can facilitate the exchange of knowledge, promote innovative approaches to management, and ultimately improve the lives of individuals living with both RLS and chronic illnesses.
In conclusion, Restless Legs Syndrome (RLS) has been found to be associated with various chronic illnesses across different medical specialties. The bidirectional relationship between RLS and chronic illnesses suggests shared risk factors, biological pathways, and possible mechanisms linking these conditions. Managing RLS symptoms in individuals with chronic illnesses can present unique challenges, requiring a comprehensive and multidisciplinary approach. By improving awareness, recognizing symptoms, and implementing appropriate treatment strategies, healthcare professionals can enhance the overall well-being and quality of life of individuals affected by both RLS and chronic illnesses. Future research and interdisciplinary collaborations hold promise for advancing our understanding and management of these complex conditions.