In this article, you will explore the intriguing relationship between sleep apnea and diabetes management. As you delve into the topic, you will discover how sleep apnea can significantly impact the effective management of diabetes. By understanding this connection, you will gain valuable insights into the importance of addressing sleep apnea as an integral part of diabetes care. So, get ready to uncover the vital link between sleep apnea and diabetes management, and how it can have a profound impact on your overall health and well-being.
Understanding Sleep Apnea
What is sleep apnea?
Sleep apnea is a common sleep disorder characterized by pauses in breathing or shallow breathing during sleep. These pauses can last for a few seconds to minutes and may occur multiple times throughout the night. This disruption in breathing can lead to a decrease in oxygen levels and an increase in carbon dioxide levels in the blood, causing the brain to briefly wake up to restore normal breathing. These frequent disruptions can result in poor quality sleep and leave you feeling tired and fatigued during the day.
Types of sleep apnea
There are three main types of sleep apnea: obstructive sleep apnea (OSA), central sleep apnea (CSA), and complex sleep apnea syndrome (CSAS).
-
Obstructive sleep apnea (OSA) is the most common type and occurs when the muscles in the back of the throat fail to keep the airway open during sleep. This blockage can be caused by the relaxation of these muscles or by physical abnormalities in the airway, such as enlarged tonsils or a deviated septum.
-
Central sleep apnea (CSA) is less common and is caused by a failure of the brain to transmit the proper signals to the muscles that control breathing. Unlike OSA, there is no physical blockage in the airway.
-
Complex sleep apnea syndrome (CSAS), also known as treatment-emergent central sleep apnea, occurs when someone with OSA develops central sleep apnea after continuous positive airway pressure (CPAP) therapy is initiated.
Symptoms of sleep apnea
Sleep apnea can manifest in a variety of symptoms, including:
- Loud, chronic snoring
- Episodes of choking or gasping for air during sleep
- Excessive daytime sleepiness or fatigue
- Morning headaches
- Difficulty concentrating or remembering
- Irritability or mood changes
- Restless sleep or insomnia
- Frequent nighttime awakenings to urinate
If you experience any of these symptoms, it is important to consult with a healthcare professional for proper diagnosis and treatment.
Link between Sleep Apnea and Diabetes
Prevalence of sleep apnea in diabetes patients
Research has shown a strong association between sleep apnea and diabetes. Studies have demonstrated that individuals with type 2 diabetes have a higher prevalence of sleep apnea compared to the general population. Estimates suggest that up to 80% of people with type 2 diabetes may have undiagnosed sleep apnea.
Impact of sleep apnea on diabetes management
Sleep apnea can have a significant impact on the management of diabetes. The disrupted sleep patterns and decreased oxygen levels associated with sleep apnea can contribute to insulin resistance, making it more difficult for the body to effectively use insulin to regulate blood sugar levels. This can lead to poor blood glucose control and an increased risk of developing complications associated with diabetes.
Shared risk factors
Sleep apnea and diabetes share certain risk factors, such as obesity, age, and family history. Obesity, in particular, plays a significant role in the development of both conditions. Excess weight can contribute to the narrowing of the airway, increasing the likelihood of sleep apnea, and also makes it more challenging for the body to effectively use insulin, leading to diabetes.

Negative Effects of Sleep Apnea on Diabetes
Increased insulin resistance
One of the negative effects of sleep apnea on diabetes is increased insulin resistance. When the body does not get enough quality sleep due to sleep apnea, it can result in higher levels of hormones that promote insulin resistance. This makes it harder for the body to regulate blood sugar levels, leading to higher glucose levels and an increased risk of complications associated with diabetes.
Poor blood glucose control
Sleep apnea can also hinder proper blood glucose control. The frequent disruptions in sleep caused by sleep apnea can result in daytime drowsiness and fatigue, making it difficult to adhere to healthy lifestyle habits necessary for diabetes management, such as regular exercise and meal planning. This can contribute to unstable blood sugar levels and make it harder to achieve optimal glucose control.
Worsening diabetic complications
Another negative effect of sleep apnea on diabetes is the potential for worsening diabetic complications. Sleep apnea has been linked to an increased risk of cardiovascular disease, stroke, and neuropathy, which are already common complications associated with diabetes. The combination of sleep apnea and diabetes can amplify the risk of these complications and accelerate their progression.
How Sleep Apnea Affects Diabetes Management
Interference with lifestyle modifications
Managing diabetes requires individuals to make certain lifestyle modifications, such as maintaining a healthy diet, engaging in regular exercise, and practicing good sleep hygiene. However, sleep apnea can interfere with these recommendations. The constant fatigue and daytime sleepiness associated with sleep apnea can make it challenging to find the motivation and energy to exercise regularly or prepare healthy meals. This can hinder diabetes management efforts.
Difficulties in medication adherence
Adherence to medication regimens is crucial for effective diabetes management. However, sleep apnea can pose difficulties in medication adherence. Fatigue and poor sleep quality can affect individuals’ overall cognitive functioning, making it harder to remember to take medications as prescribed. Additionally, the use of certain medications, such as sedatives or sleeping pills to manage sleep apnea symptoms, may interact with diabetes medications and require careful monitoring.
Challenges in blood sugar monitoring
Regular monitoring of blood sugar levels is essential for individuals with diabetes to maintain optimal glucose control. However, sleep apnea can pose challenges in blood sugar monitoring. Frequent nighttime awakenings caused by sleep apnea can disrupt sleep, making it challenging to establish a consistent routine for monitoring blood sugar levels. This inconsistency can complicate diabetes management and hinder efforts to achieve stable glucose control.

Diagnosis and Treatment of Sleep Apnea
Sleep study and screening for sleep apnea
The diagnosis of sleep apnea is typically made through a sleep study, also known as polysomnography. During a sleep study, various parameters are monitored, including brain activity, eye movements, breathing patterns, heart rate, and oxygen levels. This comprehensive evaluation allows healthcare professionals to determine the severity and type of sleep apnea present.
Additionally, screening tools, such as questionnaires or risk assessments, may be used to identify individuals who may be at higher risk for sleep apnea. These screenings can help identify individuals who may benefit from further evaluation and potential treatment.
Treatment options for sleep apnea
Treatment options for sleep apnea can vary depending on the severity and type of sleep apnea present. Conservative measures, such as weight loss, positional therapy, and avoidance of sleep-disrupting substances like alcohol or sedatives, may be recommended for milder cases or as adjunctive measures. However, for moderate to severe sleep apnea, more intensive interventions are usually necessary.
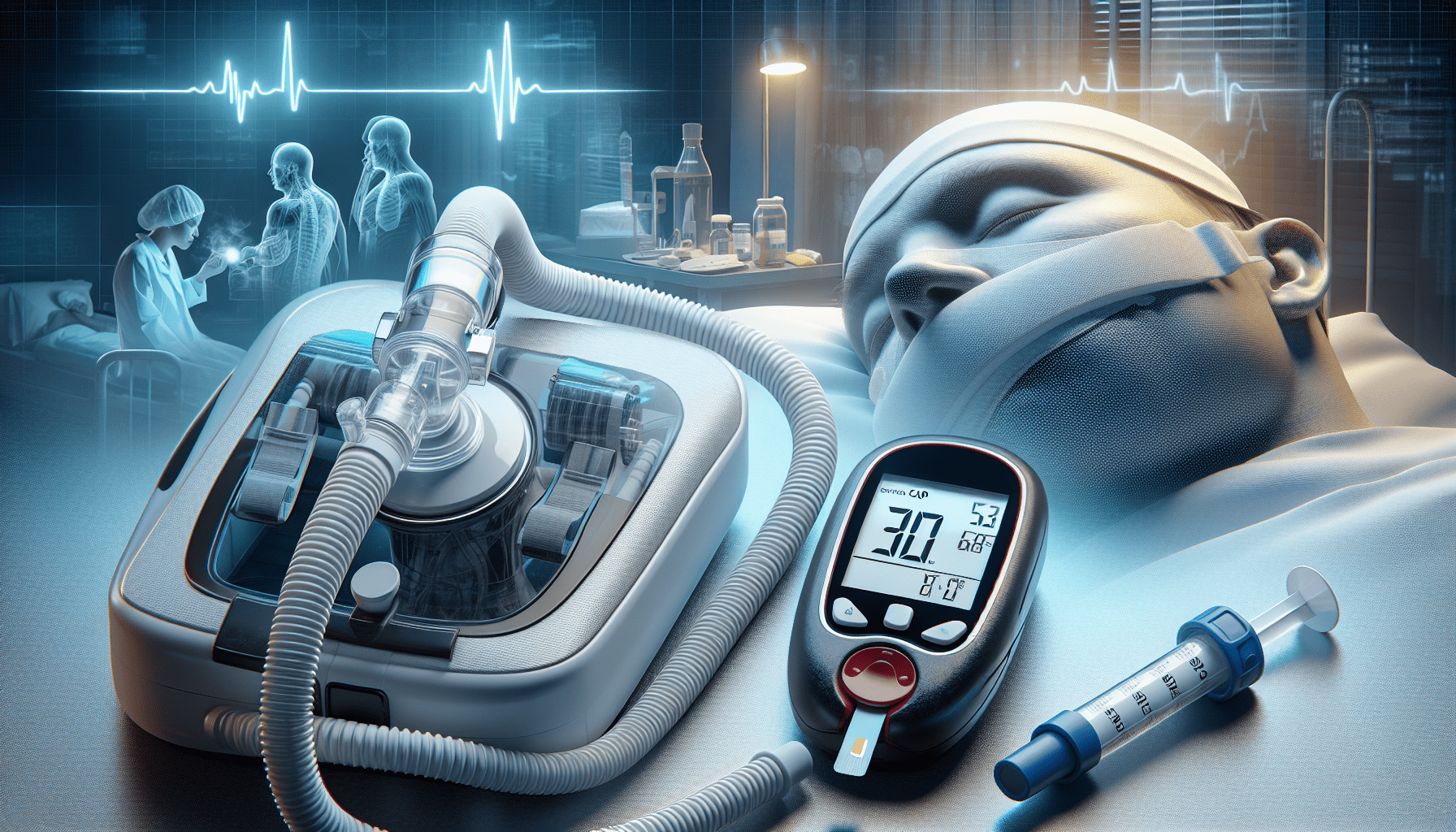
Positive airway pressure therapy
The most common and effective treatment for sleep apnea is positive airway pressure (PAP) therapy. This treatment involves wearing a mask connected to a machine that delivers a continuous flow of air pressure to keep the airway open during sleep. The most commonly used form of PAP therapy is continuous positive airway pressure (CPAP), which provides a constant level of pressure throughout the night. Other variants, such as bilevel positive airway pressure (BiPAP) and auto-adjusting positive airway pressure (APAP), may be used for individuals who require different levels of pressure support.
Impact of Sleep Apnea Treatment on Diabetes
Improved insulin sensitivity
Treating sleep apnea can have a positive impact on diabetes management. By improving the quality of sleep and reducing the frequency of breathing disruptions, sleep apnea treatment can help enhance insulin sensitivity. This can lead to improved utilization of insulin and better regulation of blood sugar levels, ultimately contributing to better overall glucose control in individuals with diabetes.
Better glycemic control
The implementation of sleep apnea treatment can also lead to better glycemic control. With improved sleep quality, individuals may experience reduced daytime drowsiness and fatigue, allowing them to adhere to their diabetes management regimen more effectively. This includes regular medication adherence, monitoring blood sugar levels as recommended, and making healthier lifestyle choices. The combination of these factors can result in more stable glucose control and reduced risk of diabetes-related complications.
Reduced risk of diabetic complications
Sleep apnea treatment has the potential to reduce the risk of diabetic complications. By improving overall sleep quality and reducing the burden of oxygen deprivation and frequent arousal, sleep apnea treatment can help mitigate some of the cardiovascular risks associated with both sleep apnea and diabetes. This may lead to a reduced risk of complications such as heart disease, stroke, and neuropathy, resulting in better long-term health outcomes for individuals with diabetes.
Integrating Sleep Apnea and Diabetes Management
Collaboration between healthcare providers
To effectively manage both sleep apnea and diabetes, collaboration between healthcare providers is crucial. A multidisciplinary approach involving physicians, sleep specialists, endocrinologists, nurses, and dietitians can ensure comprehensive care that addresses both conditions. Regular communication and coordination between these professionals can lead to more tailored treatment plans and better overall outcomes for individuals with sleep apnea and diabetes.
Importance of patient education
Patient education plays a vital role in integrating sleep apnea and diabetes management. Individuals need to understand the relationship between the two conditions, the impact of sleep apnea on diabetes management, and the potential benefits of sleep apnea treatment. Education can empower individuals to take an active role in their care, adhere to treatment regimens, and make informed decisions about their health choices.
Individualized treatment plans
Every individual with sleep apnea and diabetes requires a customized treatment plan that considers their unique needs and circumstances. Treatment goals should encompass not only the management of sleep apnea but also the optimization of diabetes control. This may involve a combination of lifestyle modifications, medication management, and regular monitoring of both conditions. Individualized treatment plans can ensure that individuals receive the best possible care to manage both sleep apnea and diabetes effectively.
Lifestyle Modifications for Better Sleep
Maintaining a consistent sleep schedule
Establishing a consistent sleep schedule is essential for better sleep. Going to bed and waking up at the same time every day, even on weekends, can help regulate the body’s internal clock and improve overall sleep quality. It is important to prioritize getting enough sleep each night to allow for adequate rest and recovery.
Creating a sleep-friendly environment
Optimizing the sleep environment can contribute to better sleep. Ensure that your bedroom is dark, quiet, and cool, as these conditions are conducive to quality sleep. Consider using blackout curtains, earplugs, or a white noise machine if necessary. Additionally, a comfortable mattress and pillows that provide adequate support can further enhance sleep quality.
Avoiding sleep-disrupting substances
Certain substances can interfere with sleep and should be avoided, especially close to bedtime. Stimulants like caffeine or nicotine can disrupt sleep patterns and make it harder to fall asleep. Alcohol may initially make you feel sleepy but can disrupt sleep and cause frequent awakenings later in the night. It is best to limit or avoid these substances, particularly in the hours leading up to bedtime, to promote better sleep.
Tips for Managing Diabetes with Sleep Apnea
Regular exercise to improve sleep and blood sugar
Engaging in regular exercise can have dual benefits for individuals with both sleep apnea and diabetes. Exercise can help improve sleep quality by promoting relaxation and reducing anxiety. Additionally, physical activity can enhance insulin sensitivity, making it easier for the body to utilize insulin and regulate blood sugar levels. Incorporating a mix of aerobic exercises, strength training, and flexibility exercises into your routine can contribute to better sleep and glucose control.
Meal planning and balanced diet
Proper meal planning and following a balanced diet are crucial components of diabetes management. When managing diabetes with sleep apnea, it is essential to pay attention to the timing and composition of meals to support optimal sleep and glucose control. Avoid heavy meals close to bedtime, as they can cause discomfort and difficulty sleeping. Focus on consuming a variety of nutrient-dense foods, including whole grains, lean proteins, fruits, vegetables, and healthy fats, to maintain stable blood sugar levels.
Managing stress to improve sleep quality
Stress can have a significant impact on both sleep and diabetes management. Finding effective stress management techniques, such as relaxation exercises, mindfulness, or engaging in enjoyable hobbies, can help improve sleep quality. By reducing stress levels, individuals can experience better sleep and ultimately enhance their ability to manage both sleep apnea and diabetes.
Conclusion
Recognizing the impact of sleep apnea on diabetes is crucial for individuals with both conditions. Sleep apnea can negatively affect diabetes management by increasing insulin resistance, hindering blood glucose control, and worsening diabetic complications. However, through diagnosis, treatment, and comprehensive management strategies, individuals can achieve better control of both sleep apnea and diabetes.
Early detection and treatment of sleep apnea are essential to minimize the negative effects on diabetes management. Improved insulin sensitivity, better glycemic control, and reduced risk of diabetic complications can be achieved through sleep apnea treatment. Collaboration between healthcare providers, patient education, and individualized treatment plans can optimize the integration of sleep apnea and diabetes management.
Additionally, lifestyle modifications, such as maintaining a consistent sleep schedule, creating a sleep-friendly environment, and avoiding sleep-disrupting substances, can promote better sleep. Combined with tips for managing diabetes with sleep apnea, including regular exercise, meal planning, and stress management, individuals can enhance their overall sleep quality and diabetes management.
By understanding the link between sleep apnea and diabetes and implementing appropriate interventions, individuals can improve their quality of life and minimize the impact of both conditions on their overall health and well-being.