Are you expecting a baby and experiencing the discomfort of restless legs? If so, you’re not alone. Many pregnant women have reported restless legs syndrome (RLS), a condition characterized by the irresistible urge to move your legs due to uncomfortable sensations. This article explores the connection between RLS and pregnancy, shedding light on its causes, symptoms, and potential remedies. So, if you’re curious about how pregnancy can contribute to restless legs syndrome and what you can do to find relief, keep reading!

What is Restless Legs Syndrome (RLS)?
Definition of RLS
Restless Legs Syndrome (RLS) is a neurological disorder that is characterized by an uncontrollable urge to move the legs, particularly during periods of rest or inactivity. People with RLS often experience uncomfortable sensations in their legs such as tingling, crawling, or aching, which can only be relieved by moving the legs. This condition can significantly disrupt sleep, leading to exhaustion and daytime sleepiness.
Symptoms of RLS
The primary symptom of RLS is an irresistible urge to move the legs. This urge is often accompanied by uncomfortable sensations, such as creeping, pulling, or burning in the legs. Symptoms typically worsen in the evening or at night, which can greatly interfere with falling asleep and staying asleep. People with RLS may also experience an overwhelming urge to walk or pace to alleviate the discomfort. Additionally, some individuals may experience symptoms in their arms or other parts of the body.
Causes of RLS
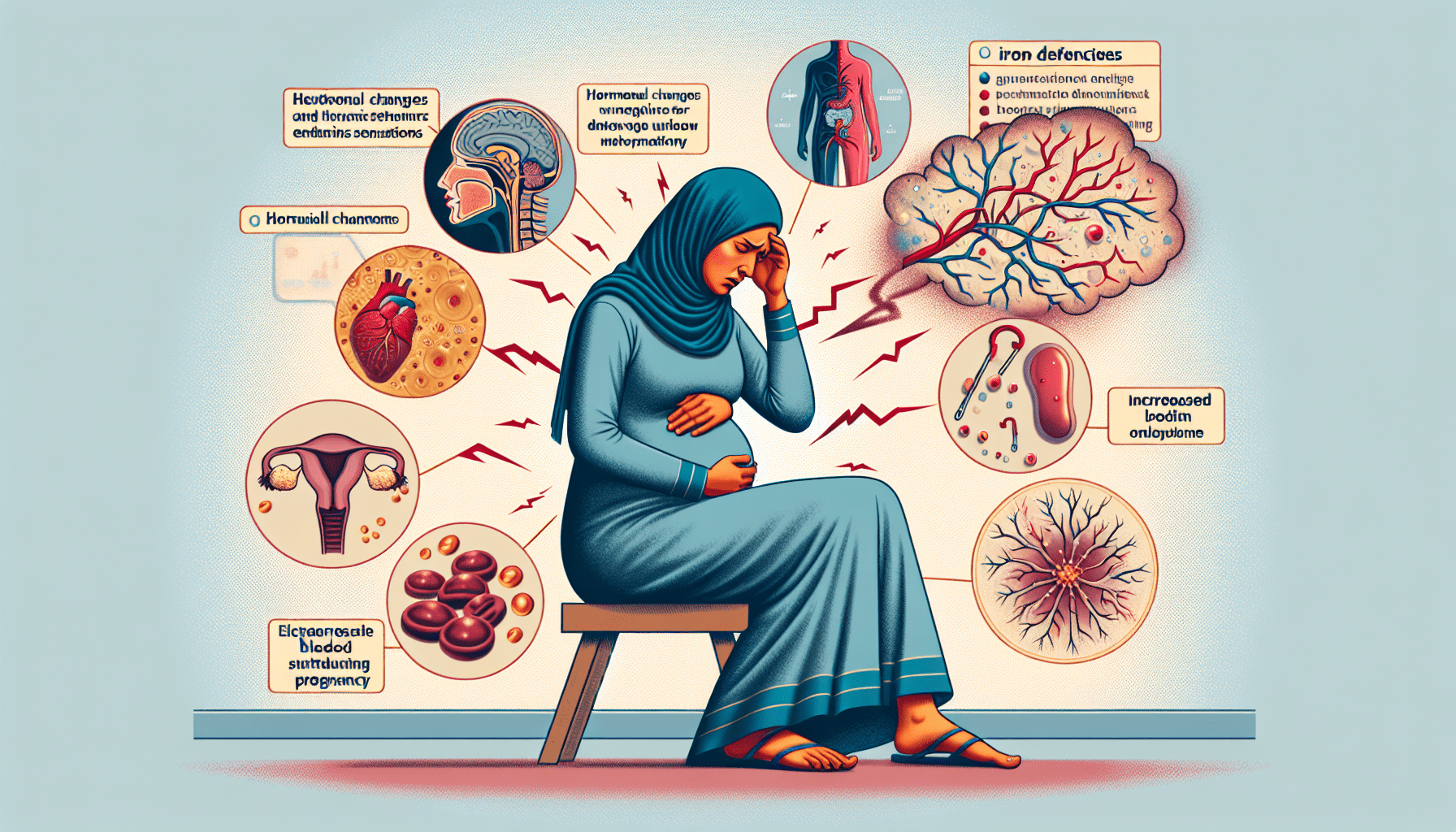
The exact cause of RLS is still unknown, but multiple factors are believed to contribute to the development of this condition. One possible cause is related to abnormalities in the dopamine levels in the brain, as dopamine plays a crucial role in regulating movement and sensations. Another contributing factor appears to be genetics, as RLS often runs in families. Certain medical conditions such as iron deficiency, kidney failure, and peripheral neuropathy have also been associated with RLS. Additionally, hormonal changes and pregnancy have been linked to an increased risk of developing RLS. Understanding these causes can help healthcare professionals develop appropriate treatments and management strategies.
Prevalence of Restless Legs Syndrome during Pregnancy
Statistics on RLS occurrence in pregnant women
Restless Legs Syndrome is relatively common during pregnancy, with studies indicating that approximately 20% of pregnant women experience RLS symptoms. This prevalence is significantly higher compared to the general population, where the occurrence of RLS is around 5-15%. The onset of RLS symptoms during pregnancy can vary, but most women experience the first symptoms in the second or third trimester.
Common trimesters for RLS symptoms
Many pregnant women who develop RLS symptoms often experience them in the second and third trimesters. This timeframe aligns with the period of rapid physical and hormonal changes that occur during pregnancy. The prevalence of RLS symptoms tends to decrease after childbirth, suggesting a relation to pregnancy hormones and physiological changes. However, it is essential to note that some women may still experience RLS symptoms even after giving birth.
Impact of Restless Legs Syndrome on Pregnancy
Effect of RLS on sleep quality
Restless Legs Syndrome can have a significant impact on the quality of sleep during pregnancy. The uncomfortable leg sensations and the overwhelming urge to move can disrupt the ability to fall asleep and maintain a restful sleep throughout the night. As a result, pregnant women with RLS often experience sleep deprivation, leading to increased fatigue, irritability, and difficulty in daily functioning. Sleep deprivation during pregnancy can also affect the overall health and well-being of both the mother and the developing baby.
Disruptive impact on daily activities during pregnancy
In addition to affecting sleep quality, Restless Legs Syndrome can disrupt daily activities for pregnant women. The constant urge to move or walk to alleviate the discomfort can make it challenging to sit or engage in activities that require prolonged periods of rest. This can interfere with work, household chores, and leisure activities, posing significant challenges to the pregnant woman’s overall well-being and quality of life.
Potential complications associated with RLS in pregnancy
While Restless Legs Syndrome itself does not pose a direct risk to the developing baby, the associated sleep disturbances and daily discomfort can have indirect consequences. Sleep deprivation during pregnancy has been linked to complications such as high blood pressure, gestational diabetes, and an increased likelihood of needing a cesarean section. Additionally, the impact of RLS on daily activities can lead to increased stress and reduced ability to engage in self-care practices, potentially affecting maternal and fetal health.
Hormonal Changes and RLS
Role of hormonal fluctuations during pregnancy
Hormonal fluctuations are a significant factor contributing to the development and exacerbation of Restless Legs Syndrome during pregnancy. The levels of certain hormones, including estrogen and progesterone, increase dramatically throughout pregnancy. These hormones play a crucial role in regulating sleep patterns, body temperature, and muscle function. However, the exact mechanisms by which these hormonal changes trigger or worsen RLS symptoms are not yet fully understood.
Link between hormone levels and RLS symptoms
Research has suggested a correlation between the presence and severity of RLS symptoms and hormonal shifts during pregnancy. Higher estrogen and progesterone levels have been associated with increased RLS symptoms, particularly during the later stages of pregnancy. These hormones may affect the dopaminergic system in the brain, disrupting the balance of neurotransmitters involved in leg movement and sensations. Further studies are needed to fully understand the intricate relationship between hormones and RLS symptoms, but this link provides valuable insights for managing and treating RLS in pregnant women.
Iron Deficiency and RLS
Relationship between low iron levels and RLS
Iron deficiency is known to be a contributing factor to Restless Legs Syndrome, both in the general population and during pregnancy. Studies have shown that individuals with low iron levels are more likely to experience RLS symptoms. Iron plays a crucial role in various bodily functions, including the production of dopamine, which is essential for proper muscle function and movement. When iron levels are depleted, dopamine production may be impaired, leading to the development or worsening of RLS symptoms.
Importance of iron for pregnant women
Iron is particularly important during pregnancy due to increased blood volume and the demands of the developing baby. Iron deficiency during pregnancy, known as iron-deficiency anemia, can have significant consequences for both the mother and the baby. It can increase the risk of preterm birth, low birth weight, and developmental delays in the baby. Therefore, maintaining adequate iron levels is crucial for the overall health and well-being of pregnant women.
Treatment options for iron deficiency-related RLS
If Restless Legs Syndrome during pregnancy is associated with iron deficiency, iron supplementation may be recommended. Iron supplements can help correct iron levels and alleviate RLS symptoms. However, it is essential to consult with a healthcare professional before starting any supplements, as iron levels need to be carefully monitored. Healthcare providers can perform blood tests to determine the appropriate dosage and duration of iron supplementation, ensuring optimal outcomes for both the mother and the baby.
Management and Treatment of RLS during Pregnancy
Non-pharmacological approaches for relieving RLS symptoms
Many pregnant women prefer to explore non-pharmacological approaches to manage and alleviate Restless Legs Syndrome symptoms. These approaches include lifestyle modifications, such as engaging in regular exercise and stretching routines. Gentle exercises, such as walking or swimming, can help improve blood flow and reduce leg discomfort. Additionally, practicing relaxation techniques, such as deep breathing exercises or yoga, can promote overall relaxation and relieve RLS symptoms.
Safe medication options for pregnant women with RLS
In some cases, healthcare professionals may recommend medication to manage severe RLS symptoms during pregnancy. However, the safety of certain medications during pregnancy is a primary concern. Medications such as opioids or sedatives are generally avoided due to potential risks to the developing baby. Instead, medications such as certain antidepressants or anti-seizure drugs may be considered, as they have shown some evidence of effectiveness in treating RLS symptoms and carrying a lower risk of adverse effects. It is crucial to consult with a healthcare professional to weigh the potential benefits and risks of medication use during pregnancy.
Consulting with healthcare professionals for personalized treatment plans
Every pregnant woman’s experience with Restless Legs Syndrome is unique, and treatment plans should be tailored to individual needs. It is essential to consult with a healthcare professional experienced in managing RLS during pregnancy. They can assess the severity of symptoms, evaluate any underlying causes, and develop a personalized treatment plan that considers the specific needs and concerns of the pregnant woman. Regular follow-up appointments are necessary to monitor progress, reassess symptoms, and make any necessary adjustments to the treatment plan.
Lifestyle Modifications to Alleviate RLS Symptoms
Exercise and stretching routines
Regular exercise is highly beneficial for managing Restless Legs Syndrome during pregnancy. Engaging in activities such as walking, swimming, or prenatal yoga can improve blood flow and promote relaxation. Stretching exercises, particularly targeting the legs, can help alleviate discomfort and reduce the frequency and severity of RLS symptoms. It is important to consult with a healthcare professional or a certified prenatal exercise instructor to develop a safe and appropriate exercise routine that takes into account individual physical capabilities and any underlying medical conditions.
Maintaining a balanced diet and proper hydration
A balanced diet rich in essential nutrients, including iron and other minerals, is crucial for managing RLS symptoms during pregnancy. Foods such as lean meats, leafy green vegetables, nuts, and legumes can help maintain optimal iron levels. It is also important to stay properly hydrated, as dehydration can exacerbate RLS symptoms. Drinking an adequate amount of water throughout the day can help prevent leg discomfort associated with RLS.
Effective sleep hygiene practices
Establishing a consistent bedtime routine and practicing good sleep hygiene can significantly improve sleep quality for pregnant women with RLS. Creating a relaxing environment, such as keeping the bedroom cool, dark, and quiet, can promote restful sleep. Avoiding stimulating activities, such as electronic device use or watching television close to bedtime, can help prepare the body for sleep. Additionally, maintaining a regular sleep schedule, even on weekends, can help regulate the body’s internal clock and promote better sleep patterns.
Alternative Therapies for Restless Legs Syndrome
Acupuncture and acupressure
Acupuncture and acupressure are ancient therapeutic practices that involve the application of fine needles or pressure on specific points of the body. These techniques have shown promise in reducing the severity of RLS symptoms and improving sleep quality. However, it is essential to consult with a trained healthcare professional who specializes in prenatal acupuncture or acupressure to ensure safety during pregnancy.
Massage therapy
Massage therapy can provide relief for pregnant women with RLS by promoting relaxation, improving circulation, and reducing muscle tension. Gentle massages targeting the legs can help alleviate discomfort and improve sleep quality. It is crucial to seek the services of a certified prenatal massage therapist who is knowledgeable about the specific needs and considerations of pregnant women.
Relaxation techniques
Practicing relaxation techniques, such as deep breathing exercises, guided imagery, or progressive muscle relaxation, can help pregnant women with RLS manage stress and promote overall relaxation. These techniques can be done independently or with the guidance of a certified instructor or through audio recordings specifically designed for pregnancy. Incorporating relaxation techniques into daily routines can be beneficial in reducing the frequency and severity of RLS symptoms.
Support and Coping Strategies for Pregnant Women with RLS
Joining support groups or online communities
Connecting with other pregnant women dealing with the challenges of Restless Legs Syndrome can provide valuable support and reassurance. Joining support groups or online communities dedicated to RLS during pregnancy can offer a safe space to share experiences, exchange coping strategies, and receive empathy and understanding. Hearing others’ stories and knowing that one is not alone in their journey can be immensely comforting and empowering.
Seeking emotional and practical support from loved ones
Pregnancy can be an emotionally and physically demanding time, especially for those experiencing Restless Legs Syndrome. Seeking support from loved ones, whether it is emotional support or practical assistance with daily tasks, can help alleviate stress and reduce the impact of RLS symptoms. Having a strong support system can provide comfort, encouragement, and relief during challenging times. Open communication with partners, family members, and close friends about RLS symptoms and the specific support needed can foster a sense of understanding and solidarity.
Coping mechanisms to manage stress and anxiety related to RLS
Dealing with Restless Legs Syndrome during pregnancy can often be accompanied by stress and anxiety. Managing stress and anxiety can contribute to better overall well-being and potentially alleviate RLS symptoms. Engaging in activities that promote relaxation, such as listening to calming music, practicing mindfulness or meditation, or engaging in hobbies and interests, can help distract from discomfort and reduce stress levels. Seeking professional counseling or therapy can also be beneficial for addressing the emotional challenges associated with RLS during pregnancy and developing effective coping strategies.
Postpartum Resolution of Restless Legs Syndrome
Natural improvement of RLS symptoms after childbirth
For many pregnant women, Restless Legs Syndrome symptoms improve or resolve after giving birth. The hormonal fluctuations that occur during pregnancy gradually normalize, and the associated physiological changes revert to their pre-pregnancy state. As a result, RLS symptoms often diminish, and sleep quality improves naturally. However, it is important to note that individual experiences may vary, and some women may continue to experience RLS symptoms after childbirth.
Continuing symptoms and possible underlying causes
While many women experience a resolution of RLS symptoms postpartum, some may continue to have symptoms. In such cases, it is important to explore potential underlying causes that may contribute to ongoing RLS symptoms. Factors such as iron deficiency, hormone imbalances, or other medical conditions should be assessed and addressed accordingly. Women experiencing persistent RLS symptoms should consult with their healthcare provider for further evaluation and appropriate management strategies.
Follow-up care and monitoring for long-term management
After childbirth, it is essential to prioritize follow-up care and monitoring for long-term management of Restless Legs Syndrome. Regular check-ups with a healthcare professional can help track symptom patterns, identify any underlying causes, and adjust treatment plans accordingly. Women who continue to experience RLS symptoms postpartum may benefit from ongoing support, education, and access to resources to effectively manage their condition. With the appropriate care and management, women can maintain a comprehensive approach to RLS and optimize their well-being both during and after pregnancy.
In conclusion, Restless Legs Syndrome can significantly impact pregnant women, affecting their sleep quality, daily activities, and overall well-being. Understanding the link between RLS and pregnancy, including the role of hormonal changes and iron deficiency, is important for effective management and treatment strategies. With a comprehensive approach that includes lifestyle modifications, alternative therapies, and support systems, pregnant women can navigate RLS symptoms and find relief. Postpartum resolution of RLS symptoms is common but not guaranteed, and ongoing follow-up care is crucial for long-term management. By prioritizing self-care, seeking appropriate support, and working closely with healthcare professionals, pregnant women can find relief and promote a healthy and enjoyable pregnancy experience.