If you’ve ever wondered why you wake up feeling tired or if you suspect that you may have a sleep disorder, then it’s time to learn about sleep studies and diagnostics. These medical tests are designed to analyze your sleep patterns, identify potential issues, and provide invaluable insights into your overall sleep health. From overnight monitoring to the measurement of brain activity, heart rate, and breathing, sleep studies can provide a wealth of information that can help you make informed decisions about your sleep and well-being. So, whether you’re struggling with insomnia, sleep apnea, or simply want to optimize your sleep quality, read on to discover what you need to know about sleep studies and diagnostics.
What is a Sleep Study?
Definition
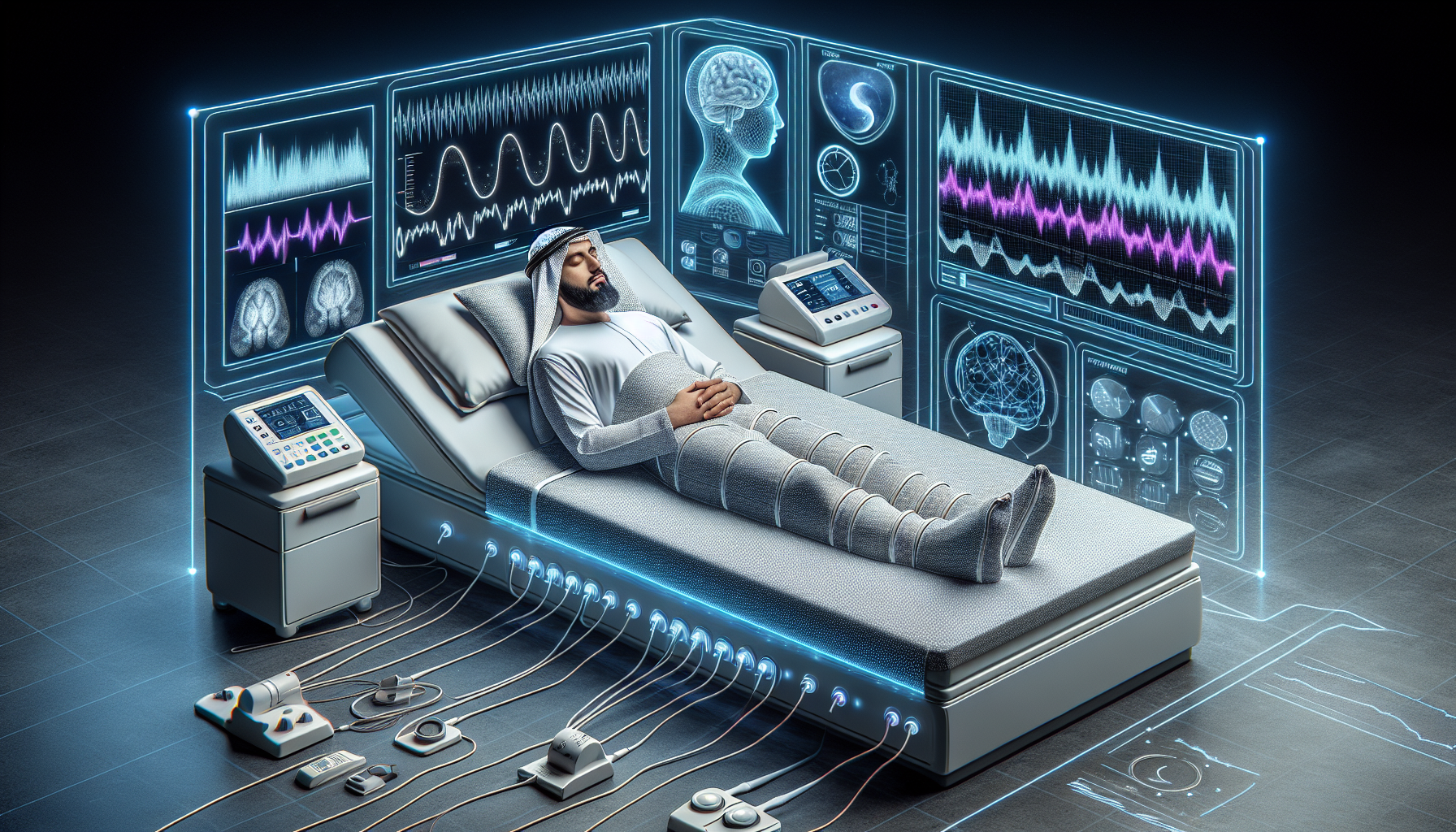
A sleep study, also known as a polysomnography, is a non-invasive diagnostic test that measures various physiological parameters while you sleep. It is conducted in a sleep laboratory to evaluate the quality and quantity of your sleep, as well as to diagnose any potential sleep disorders or conditions.
Purpose
The main purpose of a sleep study is to gather detailed information about your sleep patterns and behaviors. By monitoring your brain activity, eye movements, heart rate, breathing, and other important factors, sleep specialists can gain valuable insights into your sleep architecture and identify any abnormalities or disruptions. This information is crucial in determining the appropriate treatment plan for any sleep-related conditions you may have.
Types of Sleep Studies
There are several different types of sleep studies, each designed to focus on specific aspects of sleep. The most common types include:
-
Polysomnography (PSG): This comprehensive study records a wide range of physiological measurements, including brain waves, eye movements, muscle activity, breathing patterns, and heart rate.
-
Multiple Sleep Latency Test (MSLT): This test measures how quickly you fall asleep and assesses your level of daytime sleepiness. It is often used to diagnose narcolepsy.
-
Maintenance of Wakefulness Test (MWT): This test measures your ability to stay awake and alert during situations that typically induce sleep, such as dim lighting or sitting quietly. It is commonly used to evaluate individuals with occupations that require high levels of alertness, such as airline pilots or truck drivers.
Who Should Have a Sleep Study?
Symptoms and Conditions
Sleep studies are recommended for individuals who experience various symptoms and conditions that could signify underlying sleep disorders. Some common indicators for a sleep study include:
- Excessive daytime sleepiness
- Loud snoring, gasping, or choking during sleep
- Frequent awakenings throughout the night
- Restless leg syndrome or periodic limb movement disorder
- Episodes of stopping breathing during sleep (sleep apnea)
- Insomnia or difficulty falling asleep or staying asleep
If you experience any of these symptoms or have been diagnosed with a sleep disorder, it is important to discuss the possibility of a sleep study with your healthcare provider.
Screening Process
Before undergoing a sleep study, you will typically need to undergo a screening process to determine if you are a suitable candidate. This process may involve a comprehensive medical history review, physical examination, and completion of questionnaires or surveys related to your sleep patterns and behaviors. Your healthcare provider will then consider this information to determine if a sleep study is necessary.

Preparing for a Sleep Study
Consultation
Prior to your sleep study, you will have a consultation with a sleep specialist to discuss your sleep concerns, medical history, and any relevant medications or treatments you are currently undergoing. This consultation is an opportunity for you to ask any questions you may have and to ensure that you fully understand the purpose and process of the sleep study.
Instructions
In the days leading up to your sleep study, you will receive specific instructions regarding your preparation. These instructions may include:
- Limiting caffeine intake in the afternoon and evening of the study.
- Avoiding napping on the day of the study.
- Following your regular sleep routine as closely as possible.
- Showering before the study to ensure clean electrode application.
- Bringing comfortable sleepwear and personal hygiene items.
It is important to carefully follow these instructions to ensure accurate and reliable sleep study results.
What to Bring
When going for a sleep study, it is important to pack a few essential items to ensure your comfort and ease during the process. Some items to consider bringing include:
- Comfortable sleepwear and pajamas
- Toiletries and personal hygiene items (toothbrush, toothpaste, etc.)
- Medications you regularly take
- Any sleep aids or devices you use at home (such as CPAP machines)
Bringing these items will help create a more familiar and comfortable environment, promoting better sleep quality during the study.
What to Expect During a Sleep Study
Arrival and Set-Up
Upon arrival at the sleep laboratory, you will be greeted by a sleep technician who will guide you through the process. The technician will explain the study procedures, answer any questions you may have, and ensure your comfort throughout the night. They will then proceed with the set-up process, which involves placing various sensors and electrodes on your body to monitor different physiological parameters.
Monitoring Equipment
During a sleep study, various pieces of monitoring equipment will be used to collect data about your sleep. These may include:
- Electroencephalogram (EEG): Measures brain wave activity.
- Electrooculogram (EOG): Tracks eye movements.
- Electromyogram (EMG): Records muscle activity.
- Electrocardiogram (ECG): Monitors heart rate and rhythm.
- Pulse oximeter: Measures oxygen levels in the blood.
- Nasal airflow and respiratory effort sensors: Record breathing patterns.
- Audio and video recording devices: Document any significant events during sleep.
These devices are painless and non-invasive, and the sleep technician will ensure that they are properly applied and adjusted for optimal data collection.
Sleep Environment
The sleep laboratory is specifically designed to provide a comfortable and sleep-friendly environment. The room is typically dimly lit and equipped with a comfortable bed and bedding to replicate a home-like setting. Additionally, the temperature, humidity, and noise levels will be regulated to promote optimal sleep conditions.
Sleeping Positions
During the sleep study, you are encouraged to sleep in your preferred position. However, if the study is specifically aimed at evaluating sleep apnea, you may be asked to sleep on your back. The sleep technician will provide guidance and support in finding a comfortable position that allows for accurate data collection.

Common Sleep Study Procedures
Polysomnography (PSG)
Polysomnography is the most comprehensive type of sleep study. It involves monitoring a wide range of physiological parameters, including brain wave activity, eye movements, muscle activity, breathing patterns, and heart rate. This type of study is commonly used to diagnose sleep disorders such as sleep apnea, narcolepsy, and insomnia.
Multiple Sleep Latency Test (MSLT)
The Multiple Sleep Latency Test measures how quickly you fall asleep in a controlled environment during the day. It is typically conducted immediately after a polysomnography to assess your level of daytime sleepiness and to aid in diagnosing narcolepsy.
Maintenance of Wakefulness Test (MWT)
The Maintenance of Wakefulness Test assesses your ability to stay awake and alert during situations that typically induce sleep. It is commonly used to evaluate individuals who require high levels of alertness in their daily lives, such as airline pilots or truck drivers. This test is often conducted following a polysomnography.
Interpreting Sleep Study Results
Sleep Stages and Cycles
The sleep study results provide valuable information about the various stages and cycles of your sleep. These stages include non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. The data collected during the study allows sleep specialists to determine the amount of time spent in each stage and identify any disruptions or abnormalities.
Respiratory Events
Sleep study results can also indicate the presence and severity of respiratory events, such as snoring, pauses in breathing, and sleep apnea. These events are carefully analyzed to determine their frequency, duration, and impact on your overall sleep quality.
Movement Disorders
Some sleep disorders involve abnormal movements during sleep, such as restless leg syndrome or periodic limb movement disorder. Sleep study results can help identify these movements and assess their impact on your sleep quality.
Sleep Apnea Severity
One of the main purposes of a sleep study is to diagnose and determine the severity of sleep apnea. The results provide valuable information about the frequency and duration of breathing disruptions during sleep, allowing sleep specialists to classify the severity of sleep apnea and determine the appropriate treatment plan.
Benefits and Risks of Sleep Studies
Benefits
Sleep studies offer numerous benefits to individuals struggling with sleep-related issues. Some key benefits include:
- Accurate diagnosis: Sleep studies provide comprehensive and accurate data that helps healthcare providers accurately diagnose sleep disorders and understand their underlying causes.
- Personalized treatment plans: The results of a sleep study guide the development of personalized treatment plans tailored to address your specific sleep-related concerns.
- Improved overall health and well-being: Effective treatment based on sleep study results can lead to improved sleep quality and better overall health, including reduced daytime sleepiness, improved cognitive function, and enhanced quality of life.
Risks and Side Effects
Sleep studies are generally safe and have minimal risks or side effects. The equipment used is non-invasive and designed for comfort. Some individuals may experience minor skin irritation from the adhesive used to attach the electrodes, but this is typically temporary and easily treated. It is important to discuss any concerns or potential risks with your healthcare provider before undergoing a sleep study.
Treatment Options Based on Sleep Study Results
Non-Invasive Treatments
The treatment options for sleep disorders vary depending on the specific diagnosis from the sleep study. Non-invasive treatments may include:
- Improving sleep hygiene: Making lifestyle changes such as establishing consistent sleep routines, creating a comfortable sleep environment, and avoiding electronic devices before bed.
- Cognitive-behavioral therapy: This therapy focuses on addressing the underlying psychological and behavioral factors contributing to sleep problems.
- Light therapy: Used to regulate sleep-wake cycles, particularly in individuals with circadian rhythm sleep disorders.
Continuous Positive Airway Pressure (CPAP)
CPAP is a common treatment for obstructive sleep apnea. It involves wearing a mask over the nose or mouth during sleep, which delivers a continuous stream of pressurized air to keep the airway open and prevent pauses in breathing.
Oral Appliances
Oral appliances, such as dental devices, may be recommended for individuals with sleep apnea or snoring. These devices help maintain an open airway by repositioning the jaw or tongue during sleep.
Surgical Interventions
In some cases, surgical interventions may be necessary to address anatomical abnormalities contributing to sleep disorders. Procedures such as uvulopalatopharyngoplasty (UPPP), tonsillectomy, or nasal surgery may be recommended to improve airway function and alleviate sleep-related symptoms.
Costs and Insurance Coverage
Insurance Approval
Before scheduling a sleep study, it is important to check with your insurance provider to understand the coverage and authorization process. Many insurance plans require pre-approval or a referral from a primary care physician before covering the costs of a sleep study.
Out-of-Pocket Costs
The total cost of a sleep study can vary depending on factors such as the location of the sleep laboratory and the specific type of study being conducted. In general, sleep studies can range from a few hundred to several thousand dollars. It is advisable to check with your healthcare provider and insurance company to determine your expected out-of-pocket expenses.
Reimbursement Options
If you incur out-of-pocket expenses for a sleep study, there may be reimbursement options available. These can include submitting claims to your insurance provider or utilizing flexible spending accounts (FSAs) or health savings accounts (HSAs) if eligible.
Conclusion
Sleep studies play a crucial role in diagnosing and treating sleep disorders. By monitoring various physiological parameters during sleep, these studies provide valuable insights into your sleep architecture and help healthcare providers develop personalized treatment plans. If you are experiencing sleep-related symptoms or have been diagnosed with a sleep disorder, discussing the possibility of a sleep study with your healthcare provider can provide the necessary guidance and support to improve your sleep quality and overall well-being.