Have you ever wondered why you wake up feeling tired and groggy, despite getting a full night’s sleep? It could be due to sleep apnea, a common sleep disorder that affects millions of people worldwide. In this article, we will explore the different types of sleep apnea and help you understand the variations, so you can better identify and address any issues you may have been experiencing. Whether you are a snorer or have been feeling exhausted during the day, this article will shed light on the different types of sleep apnea and provide you with valuable insights to improve your sleep quality and overall well-being.
Obstructive Sleep Apnea
Definition
Obstructive Sleep Apnea (OSA) is a sleep disorder characterized by repeated episodes of partial or complete blockage of the upper airway during sleep. This obstruction causes a disruption in breathing, leading to a decrease in oxygen levels in the blood and subsequent arousal from sleep. OSA is the most common type of sleep apnea, affecting millions of people worldwide.
Causes
The primary cause of obstructive sleep apnea is the relaxation or collapse of the muscles in the throat, blocking the airway. This relaxation can occur due to a variety of factors, including obesity, excess fat deposition around the neck and throat, anatomical abnormalities like a deviated septum or narrow airway, large tonsils or adenoids, and certain medical conditions like hypothyroidism or acromegaly.
Symptoms
The most common symptoms of obstructive sleep apnea include loud snoring, excessive daytime sleepiness, pauses in breathing during sleep, choking or gasping sensations during sleep, restless sleep, morning headaches, dry mouth or sore throat upon waking, difficulty concentrating, and irritability. It is important to note that not all individuals with OSA experience the same symptoms, and the severity can vary.
Diagnosis
To diagnose obstructive sleep apnea, a sleep study, also known as polysomnography, is conducted. This study measures several parameters during sleep, including brain activity, eye movements, heart rate, breathing patterns, and oxygen levels. The study is usually done in a sleep center, where various electrodes and sensors are used to collect data throughout the night. The results of the sleep study help in determining the presence and severity of OSA.
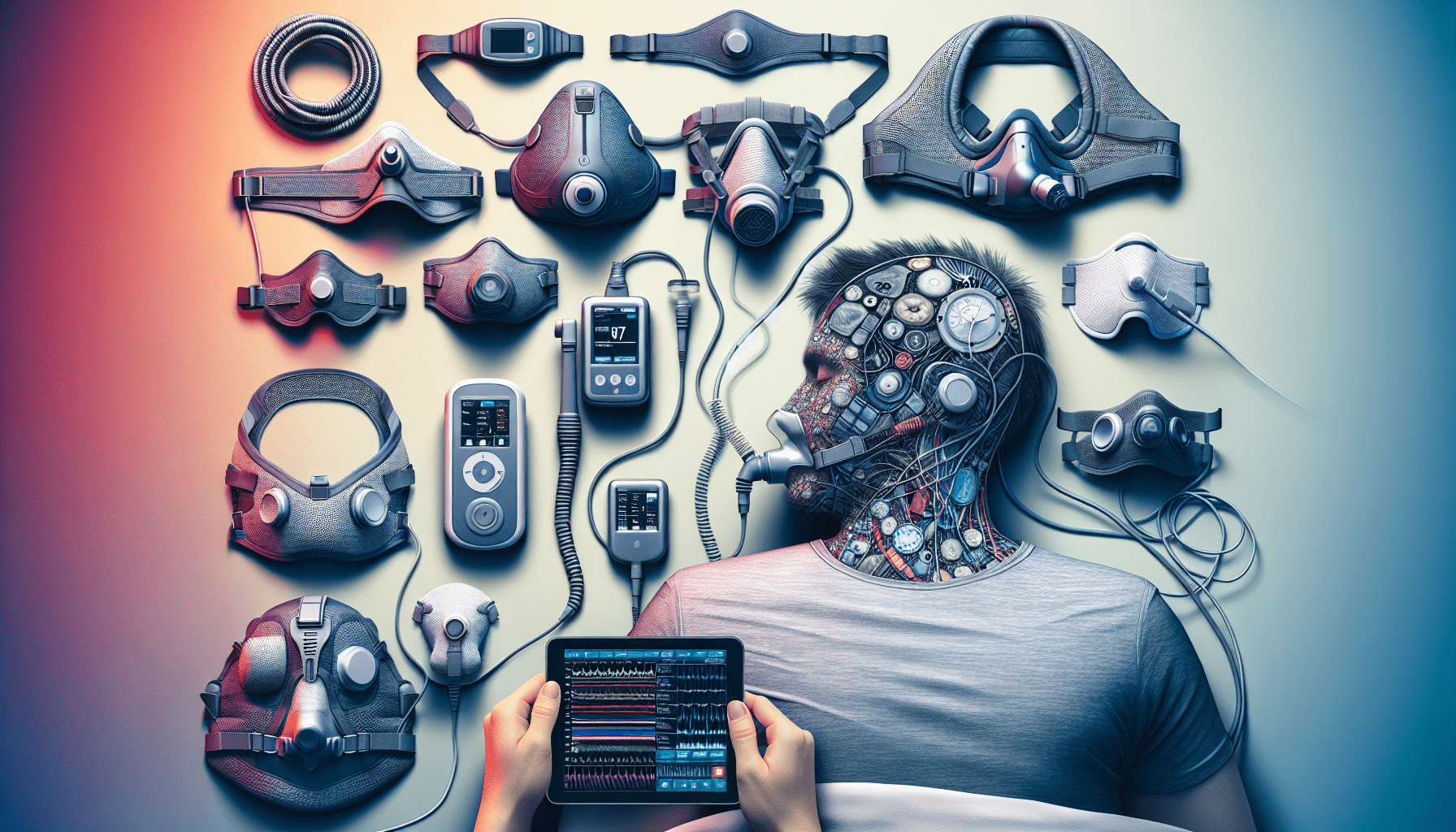
Treatment Options
Treatment options for obstructive sleep apnea depend on the severity of the condition and individual factors. Lifestyle changes such as weight loss, regular exercise, and avoiding alcohol and sedatives can help reduce symptoms. Continuous Positive Airway Pressure (CPAP) therapy is a common treatment method where a machine delivers air pressure through a mask worn over the nose or mouth, keeping the airway open during sleep. Other options include oral appliances, positional therapy, and in some cases, surgical interventions to remove obstructions or correct anatomical abnormalities.
Central Sleep Apnea
Definition
Central Sleep Apnea (CSA) is a sleep disorder characterized by a disruption in the brain’s normal signals to control breathing during sleep. Unlike obstructive sleep apnea, the airway remains open, but the brain fails to send the appropriate signals to the muscles that control breathing, leading to temporary pauses in respiration.
Causes
Central sleep apnea can occur due to various underlying conditions. It is commonly associated with certain medical conditions like heart failure, stroke, brainstem injury, or degenerative diseases like Parkinson’s disease. Certain medications, such as opioids or sedatives, can also contribute to the development of CSA. Moreover, high altitudes and breathing irregularities related to Cheyne-Stokes respiration can be causes of CSA.
Symptoms
The symptoms of central sleep apnea may include restless sleep, frequent awakenings, insomnia, morning headaches, fatigue, daytime sleepiness, difficulty concentrating, and mood changes. Unlike OSA, loud snoring is not typically associated with CSA.
Diagnosis
A sleep study is also used to diagnose central sleep apnea. In addition to measuring brain activity, eye movements, and heart rate, the study also examines the absence of breathing efforts during sleep. The specific patterns observed in the sleep study help differentiate central sleep apnea from other sleep disorders.
Treatment Options
Treatment for central sleep apnea depends on the underlying cause. Treating the primary medical condition, such as heart failure or neurological disorders, may alleviate the symptoms of CSA. Supplemental oxygen therapy, adaptive servo-ventilation (ASV), or the use of certain medications may also be prescribed to help regulate breathing during sleep.

Mixed Sleep Apnea
Definition
Mixed Sleep Apnea, also known as complex sleep apnea, is a combination of obstructive sleep apnea and central sleep apnea. It occurs when an individual experiences episodes of both partial or complete upper airway obstruction and a lack of respiratory effort during sleep.
Causes
The exact causes of mixed sleep apnea are not fully understood. It is believed to result from a combination of factors contributing to both obstructive and central sleep apnea. Some individuals may initially have OSA, which, when left untreated, can lead to the development of CSA over time.
Symptoms
The symptoms of mixed sleep apnea resemble those of both OSA and CSA. These may include loud snoring, gasping or choking during sleep, pauses in breathing, morning headaches, daytime sleepiness, mood changes, and difficulty concentrating.
Diagnosis
A sleep study is essential in diagnosing mixed sleep apnea. The study analyzes the specific patterns of obstruction and central respiratory events to confirm the presence of both components of the disorder.
Treatment Options
Treatment for mixed sleep apnea often involves a combination of approaches used for OSA and CSA. This may include lifestyle changes, weight loss, positional therapy, CPAP therapy, oral appliances, and sometimes surgical interventions. The specific treatment plan is determined based on the individual’s symptoms, severity, and underlying causes of the sleep apnea.
Complex Sleep Apnea Syndrome
Definition
Complex Sleep Apnea Syndrome is a type of sleep apnea that is characterized by the presence of central sleep apnea patterns during a continuous positive airway pressure (CPAP) titration study, even though no pre-existing central sleep apnea was evident during the diagnostic study.
Causes
The exact causes of complex sleep apnea syndrome are not fully understood. It is believed to occur primarily as a result of the initiation or persistence of central sleep apnea during CPAP therapy. The reasons behind why some individuals develop complex sleep apnea syndrome while using CPAP remain unclear.
Symptoms
The symptoms of complex sleep apnea syndrome are similar to those of central sleep apnea. They may include disrupted sleep, frequent awakenings, morning headaches, fatigue, daytime sleepiness, and mood changes.
Diagnosis
Diagnosing complex sleep apnea syndrome involves conducting a sleep study that specifically assesses the presence of central sleep apnea patterns during CPAP therapy. This study helps differentiate complex sleep apnea syndrome from other types of sleep apnea.
Treatment Options
The treatment options for complex sleep apnea syndrome can be complex and highly individualized. They may include modifications in CPAP therapy, the use of different pressure settings, oxygen supplementation, the addition of adaptive servo-ventilation (ASV), or the use of positional therapy. Close monitoring and follow-up with a sleep specialist are crucial in managing the condition effectively.

Upper Airway Resistance Syndrome
Definition
Upper Airway Resistance Syndrome (UARS) is a sleep disorder characterized by increased resistance to airflow in the upper airway during sleep, leading to disrupted breathing patterns and fragmented sleep.
Causes
The underlying causes of UARS are similar to those of obstructive sleep apnea. It can be associated with factors such as excessive relaxation of throat muscles during sleep, anatomical abnormalities in the upper airway, obesity, nasal congestion, or certain medical conditions.
Symptoms
The symptoms of UARS are similar to those of obstructive sleep apnea but often milder in intensity. These may include snoring, frequent awakenings, fatigue, excessive daytime sleepiness, morning headache, difficulty concentrating, and irritability.
Diagnosis
Diagnosing UARS involves conducting a sleep study to assess the degree of airflow resistance in the upper airway during sleep. This is typically done through the measurement of various parameters, including nasal pressure, body position, and respiratory effort.
Treatment Options
Treatment options for UARS include lifestyle modifications, weight management, avoiding alcohol and sedatives, positional therapy, and the use of oral appliances to help maintain open airways during sleep. Continuous Positive Airway Pressure (CPAP) therapy may also be prescribed in severe cases.
Nocturnal Hypoventilation Syndrome
Definition
Nocturnal Hypoventilation Syndrome (NHS) is a sleep-related breathing disorder characterized by abnormally low levels of oxygen and high levels of carbon dioxide in the blood during sleep. It occurs when there is inadequate ventilation in the lungs, leading to impaired gas exchange.
Causes
NHS can be caused by a variety of factors, including respiratory muscle weakness, conditions that affect the nervous system or chest wall, obesity, certain medications, or respiratory drive disorders. Individuals with pre-existing lung diseases, such as chronic obstructive pulmonary disease (COPD), may be more prone to developing NHS.
Symptoms
The symptoms of NHS may include excessive daytime sleepiness, morning headaches, fatigue, difficulty concentrating, poor memory, mood changes, restless sleep, and frequent awakenings.
Diagnosis
Diagnosing NHS involves conducting a sleep study to assess respiratory patterns, oxygen saturation levels, and carbon dioxide levels during sleep. Additional tests, such as arterial blood gas analysis, may also be performed to determine the blood gas levels during sleep.
Treatment Options
Treatment options for NHS depend on the underlying cause and severity of the condition. Treatments may include treating the primary medical condition, nocturnal ventilation support such as Bi-level Positive Airway Pressure (BiPAP) therapy, oxygen supplementation, or in severe cases, non-invasive positive pressure ventilation (NIPPV) or invasive ventilatory support may be necessary.
Positional Sleep Apnea
Definition
Positional Sleep Apnea is a type of sleep apnea where the severity of sleep apnea events, particularly obstructive events, is significantly greater when an individual sleeps in certain positions, typically on their back.
Causes
The exact causes of positional sleep apnea are not fully understood. However, the supine position (sleeping on the back) is known to contribute to the relaxation of throat muscles and narrowing of the upper airway, leading to increased obstruction during sleep.
Symptoms
The symptoms of positional sleep apnea are similar to those of obstructive sleep apnea, but they are more pronounced or occur exclusively when sleeping in certain positions. These symptoms may include loud snoring, excessive daytime sleepiness, pauses in breathing during sleep, choking or gasping sensations during sleep, restless sleep, morning headaches, dry mouth or sore throat upon waking, difficulty concentrating, and irritability.
Diagnosis
Positional sleep apnea is typically diagnosed through a sleep study. The study evaluates the presence and severity of sleep apnea events in different positions, particularly when an individual is sleeping in the supine position.
Treatment Options
The primary treatment for positional sleep apnea involves positional therapy, which encourages individuals to sleep in positions other than on their back. Techniques such as using positional pillows, wearing a backpack, or utilizing devices that gently vibrate or provide positional feedback can help individuals maintain a non-supine sleeping position. Other treatment options for positional sleep apnea may involve lifestyle changes, weight loss, or the use of continuous positive airway pressure (CPAP) therapy when necessary.
Idiopathic Sleep Apnea
Definition
Idiopathic Sleep Apnea (ISA) refers to sleep apnea that occurs without an identifiable underlying cause. In idiopathic cases, the exact reason for the development of sleep apnea cannot be determined.
Causes
The underlying causes of idiopathic sleep apnea remain unknown. Genetic factors, anatomical abnormalities in the upper airway, or abnormalities in how the brain controls breathing during sleep may contribute to its development.
Symptoms
The symptoms of idiopathic sleep apnea are similar to those of obstructive sleep apnea. These may include loud snoring, excessive daytime sleepiness, pauses in breathing during sleep, choking or gasping sensations during sleep, restless sleep, morning headaches, dry mouth or sore throat upon waking, difficulty concentrating, and irritability.
Diagnosis
Diagnosing idiopathic sleep apnea involves conducting a sleep study to assess the presence and severity of sleep apnea events. The study helps rule out other potential causes and confirms the presence of sleep apnea without a known underlying cause.
Treatment Options
The treatment options for idiopathic sleep apnea are similar to those used for obstructive sleep apnea. Lifestyle modifications, weight loss, avoiding alcohol and sedatives, positional therapy, and the use of continuous positive airway pressure (CPAP) therapy are common treatment approaches. Depending on the severity and individual factors, other treatments such as oral appliances or surgical interventions may also be considered.
Obesity Hypoventilation Syndrome
Definition
Obesity Hypoventilation Syndrome (OHS) is a sleep-related breathing disorder primarily associated with morbid obesity. It is characterized by reduced ventilation in the lungs, resulting in abnormally high levels of carbon dioxide in the blood during sleep.
Causes
OHS occurs due to the combined effects of obesity-related factors. Excess weight can put pressure on the chest wall, making it difficult for the respiratory muscles to expand the lungs effectively. Additionally, obesity can lead to changes in respiratory control, causing abnormal ventilation patterns during sleep.
Symptoms
The symptoms of obesity hypoventilation syndrome may include excessive daytime sleepiness, morning headaches, fatigue, difficulty concentrating, poor memory, mood changes, restless sleep, snoring, and frequent awakenings.
Diagnosis
Diagnosing OHS involves conducting a sleep study to assess respiratory patterns, oxygen saturation levels, and carbon dioxide levels during sleep. Additionally, assessment of lung function and blood tests may also be performed to evaluate respiratory and metabolic parameters.
Treatment Options
The primary treatment for obesity hypoventilation syndrome involves weight loss through a combination of lifestyle modifications such as dietary changes, increased physical activity, and behavior modifications. Supplemental oxygen therapy and non-invasive positive pressure ventilation (NIPPV) may also be utilized to improve oxygenation and ventilation during sleep. In some cases, bariatric surgery may be considered to aid in weight reduction and improve respiratory function.
Nocturia Sleep Apnea
Definition
Nocturia Sleep Apnea, also known as nocturnal polyuria sleep apnea, is a type of sleep apnea that is characterized by frequent urination during the night, leading to disrupted sleep patterns.
Causes
The exact causes of nocturia sleep apnea are not fully understood. It is believed that the changes in fluid balance and urine production during sleep contribute to the increased frequency of nighttime urination in individuals with sleep apnea.
Symptoms
The primary symptom of nocturia sleep apnea is the need to wake up multiple times during the night to urinate. This frequent urination disrupts sleep patterns, leading to daytime sleepiness, fatigue, and impaired quality of life.
Diagnosis
To diagnose nocturia sleep apnea, a sleep study is typically conducted to assess the presence and severity of sleep apnea events. Additionally, a thorough evaluation of urinary patterns and fluid intake may be necessary to evaluate the specific cause of the nocturia.
Treatment Options
Treatment options for nocturia sleep apnea may involve a combination of approaches. The use of continuous positive airway pressure (CPAP) therapy or positional therapy can help manage sleep apnea and subsequently reduce the frequency of nighttime urination. Additional interventions, such as fluid management strategies, dietary adjustments, or the use of medications, may be recommended to address the underlying cause of nocturia. It is important to consult with a healthcare professional to determine the most suitable treatment plan.